In the liver sits. Why removal of liver tumors is an indicator of the surgeon's superior skill
As part of materials on the treatment of oncological diseases, we have not touched on such a crucial area as surgery in our blog. Although it is surgical removal of the tumor - the only radical method of treatment that exists in oncology.
A radical method is one that eliminates the main problem and the cause of all other severe symptoms: a malignant neoplasm.
“Medicine 24/7” , first of all, is a surgical hospital with a serious load: among private clinics in Moscow, ours is in the first place for the consumption of blood and blood components that are necessary for operations.
Liver operations are not the most important and popular direction of the clinic. However, the fact that in our hospital, in principle, such manipulations are done, rather than sending patients somewhere else, is a marker and an indicator of the highest qualification of the surgeon’s team.
')
Operations on the liver are equivalent to operations on the brain and open heart. As a rule, this is the seventh complexity category out of 7.
At the same time, successful surgical treatment of malignant neoplasms in the liver makes it possible to count on the patient's life extension: five-year survival of 40-50% in primary liver cancer or single metastases is a good result.
We often receive patients who were not operated on at other clinics for some official reason. But people want to take a second chance, and we give it to them.
In this article we will try to explain why the liver so often requires attention in the treatment of cancer, why not every surgeon risks operating on it, and whether there are alternatives to the scalpel.
The liver is an amazingly multi-tasking organ . The work can be divided into 3 directions.
1. Depositing. In the liver, the body stores many of the necessary things: energy reserves in the form of glycogen; some vitamins (A, D, B12, K, PP); trace elements (the main of which is iron).
Also here is a very significant amount of blood. If an unforeseen hole is formed in the body as a result of the injury, then this blood reserve will be urgently thrown into the main bloodstream and will compensate for blood loss for a while.
2. Synthesis. This organ is the “factory” of important hormones and enzymes. Many plasma proteins, including those by which blood coagulates when needed, but does not stick together in blood clots in ordinary life - are formed here. But most importantly, the liver produces bile, a component of healthy digestion.
3. detox. The liver is unique in that it is able to neutralize poisons, toxins, allergens and other dangerous substances that have entered the body from the outside, as well as originated as a product of our metabolism.
All these important functions of the liver are provided by its special blood supply system.
About 1.5 liters of blood pass through the liver in a minute. About a quarter of this volume enters the hepatic artery, and the remaining 75% through the portal vein from the intestine.
There are sinusoids inside the liver - special capillaries in which arterial blood is mixed with venous blood and this mixture is already “filtered” by hepatocytes (cells of the liver tissue): useful and nutrients are stored, toxins are neutralized as a result of complex chemical reactions. Then the blood, which has passed all the stages of "treatment", enters the hepatic vein and returns to the heart.
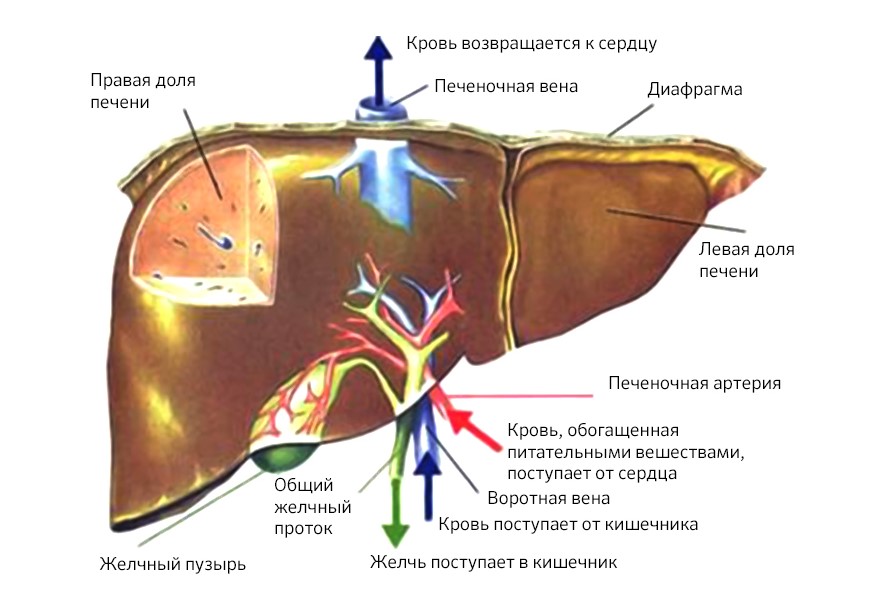
Circulation of blood in the liver
But this remarkable system, which allows the liver to filter 2,000 liters of blood per day, also contributes to the spread of cancer cells. They are carried through the body through the bloodstream, and the liver, which transmits and retains all that is superfluous, thus becomes a target for metastasis.
According to statistics, the primary liver tumor - hepatocellular carcinoma - is less common than metastases in this organ from other malignant neoplasms. The total number of patients with metastases in the liver in Russia is more than 100,000 - many times more than patients with primary tumors of the liver and intrahepatic bile ducts (less than 15,000).
But almost all malignant neoplasms metastasize to the liver. Colon cancer (colorectal cancer) does this in 50% of cases. In 30% of cases, metastatic lesions occur in melanoma and breast cancer.
Our leading oncologist surgeon in this field, Anton Aleksandrovich Ivanov, gives one of the most interesting examples in his practice.
“A patient with metastatic breast cancer in the liver. Usually such cases are not accepted to operate at all. But during the examination we found out that the liver is the only organ that has met metastasis. It was a rare success, and the surgeons made a collegial decision: to operate.
And when, in preparation for the operation, a biopsy of metastases was done, it turned out that cancer cells in the liver had mutated, and the initial HER2-negative status of the tumor changed, became HER2-positive, 3+. This means that the disease is sensitive to Herceptin, an effective remedy against this type of cancer. The patient was removed metastases, resected half of the liver. More than 10 years have passed, she receives the drug and is still alive. When she comes to the surveys, she complains not so much about her state of health, but rather of hooligans and grandchildren. ”
Unfortunately, both liver cancer and metastases in it are often diagnosed in an already neglected state.
The reasons for this situation are the reverse side of the "superpowers" of the body. The liver has a huge margin of safety: to cope with its duties, it is enough for 15-20% of a healthy parenchyma (liver tissue).
“Tumors themselves do not hurt, but simply use the healthy tissue resource. So it turns out that a liver damaged by a tumor may not give signals at all until more than half of the organ is affected by the disease - and this is stage III-IV: 58% of primary liver tumors are detected in Russia in a state of neglected process, ”explains Anton Alexandrovich .
At the same time, ultrasound and even CT can skip a node in the liver, if it is still very small, and not in 100% of cases such studies make it clear the exact size, shape and nature of the focus.
This diagnostic complexity can be overcome: use of contrast media for hepatotropic (ie, targeting the liver) MRI. Only three of them, in Russia since 2007, one has been allowed and recommended for use: Primovist. It is able to accumulate in hepatocytes, but malignant tumors do not “absorb” it, due to this they become most clearly visible in the pictures.
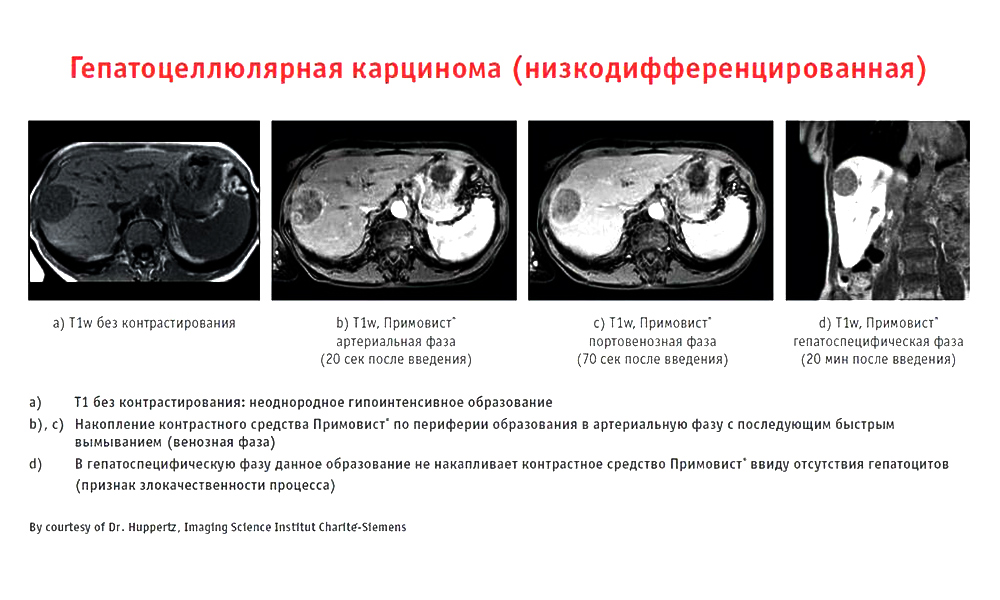
An example of the work of the contrast drug Primovist
Today, this drug is the gold standard for MRI diagnosis of liver tumors, the hepatologists in Medicine 24/7, use it without fail, which ensures an adequate level of accuracy.
But, unfortunately, in many regions the situation is more difficult: finding there clinics that know and use Primovist is still difficult, like 10 years ago.
Even finding a tumor in the liver, not every doctor will be able to remove it: it is more difficult for a surgeon to work in the hepatopancreatobiliary zone than read the word “hepatopancreatobiliary” the first time.
This zone includes the liver (Greek hepar), pancreas (lat. Pancreas), gall bladder (lat. Vesica biliaris) and bile ducts. All these organs are closely related anatomically and functionally.
Most interventions in other areas of surgery take place at one small specific location, and if we are talking about resection (removal of a part) of the liver, then the amount of work is great, even with one or two segments affected.
It is difficult, firstly, technically.
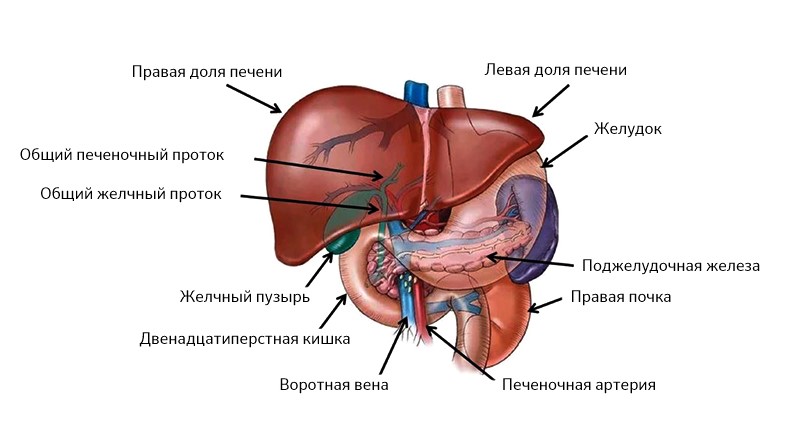
The liver is on the right side, the pancreas is on the left, all their ducts are combined into one and out into the duodenum
The liver is very complex, it consists of segments and lobes, between which there are ligaments, all of them literally enmeshed and penetrated by the veins, arteries and bile ducts.
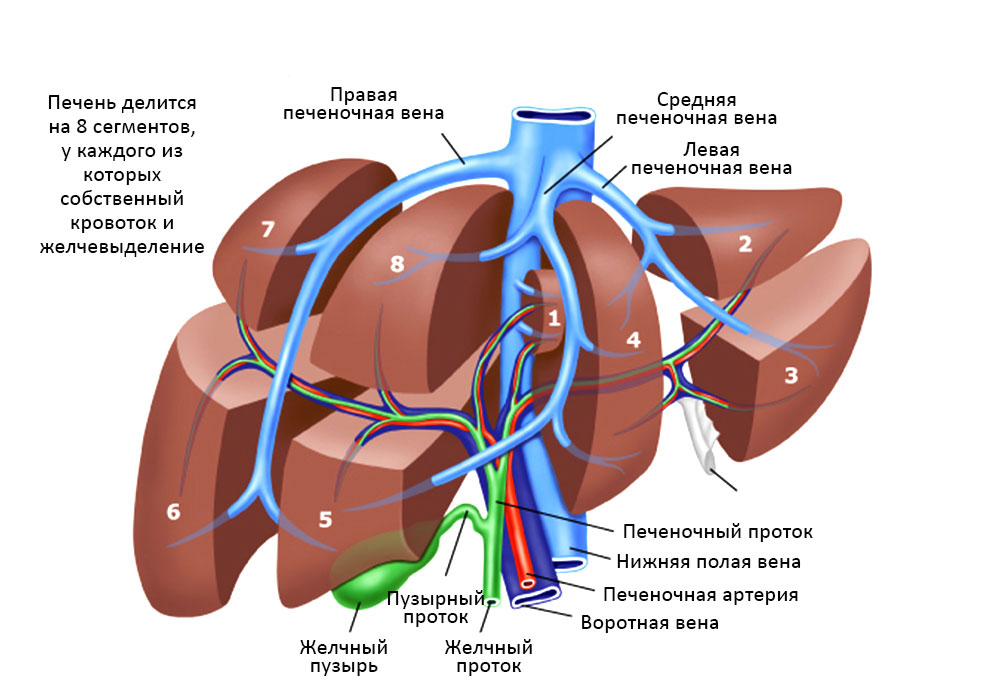
The relationship of the segments of the liver, bile ducts and blood vessels
There is a risk that a large vascular bundle is located in this area, everything happens very close to the inferior vena cava, hepatic artery: these are large great vessels. The liver itself is bleeding badly. Accordingly, there is a danger of serious blood loss, the operation should be as fast as possible and extremely accurate at the same time.
Such an intervention should be performed by a person with extensive experience in conducting these operations, and the number of such specialists goes to one. In Medicine 24/7, there are two of them at once, and patients often come to them in the direction from colleagues from other (highly respected) medical institutions, where, nevertheless, there are no specialists with sufficient skills.
Both the doctor and the patient are thoroughly prepared for liver surgery so that everything goes as predictably as possible. Anton Aleksandrovich Ivanov explained in detail how an oncologist and his team prepare for a liver surgery, and that they are trying to envisage everything.
“In order to accurately determine the scope and method of intervention, conduct all the necessary research. The area of operation is visualized with maximum accuracy. The results of multiple tests are taken into account. For example, in certain infectious diseases or a decrease in the number of platelets in the blood, the doctor will first select a therapy to restore normal parameters and only then prescribe an operation.
Immediately at the time of the intervention in the operating room, in addition to the doctor, there is a whole team of specialists monitoring the patient’s vital activities: anesthesiologists, resuscitators, transfusiologists, and an operating sister. Of course, today even the doctor does not remove the tooth alone, but liver operations collect the largest brigade in the operating room.
It is necessary to ensure the supply of blood components - erythrocyte mass, plasma, so that at any time with large blood loss it was possible to compensate for them. In our practice, we use a special device, Cell Saver, which immediately separates (separates) red blood cells from the patient’s lost blood and returns them back to its bloodstream. "Own" is always more favorable than "canned" donor erythrocytes, even suitable for the blood group. "
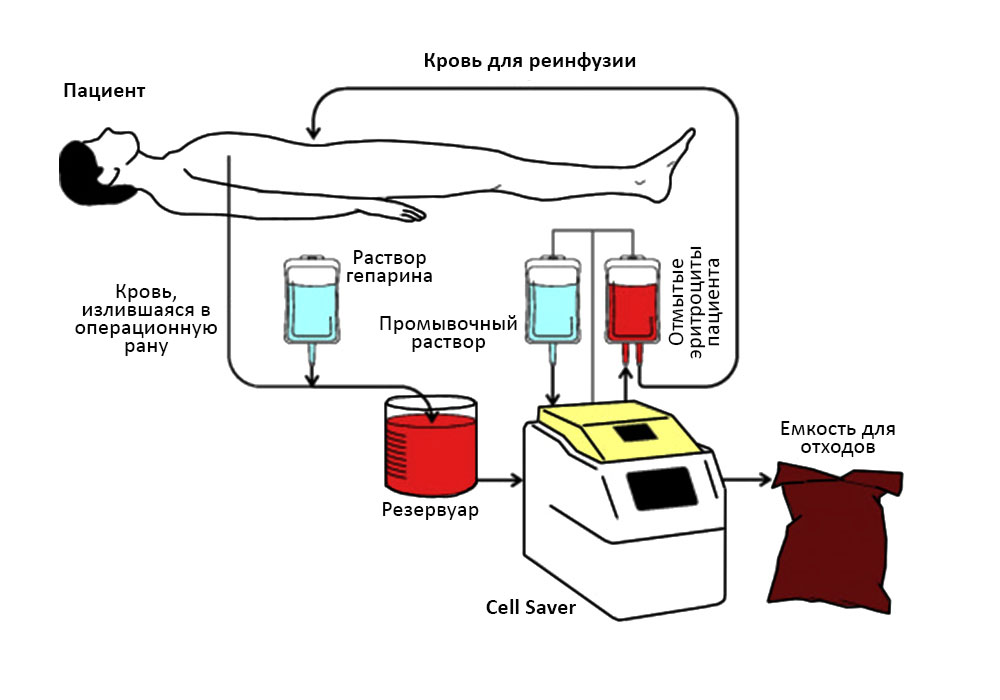
The patient’s blood enters the Cell Saver apparatus and he returns the red blood cells to the patient.
Quite regularly, surgeries are simultaneous (simultaneous): liver resection takes place simultaneously with other interventions. Removed and the primary focus, for example, in the colon, and metastasis in the liver.
However, even with maximum predictability and complete control of the process, surgeons happen to deviate from the intended plan.
For example, during surgery for a primary tumor of the stomach, an occasional find may occur: a small single metastasis in the liver. In this case, surgeons can invite colleagues, specialists in operations on the liver, so that they spend their stage: removal of a part of the liver.
Joint operations are good because the patient is subjected to anesthesia and the difficulties of the recovery period only once.
By the time the operation takes from 1.5 hours (with resection of a single metastasis) to 10-12. “In my practice, the longest operation with simultaneous removal of the primary focus in the intestine and liver metastases lasted 15 hours,” recalls Dr. Ivanov, “but this case is rather exceptional.”
Size matters. If the tumor is large, it managed to “eat” too much healthy tissue, then removing it may be meaningless. In order for the patient to have a guaranteed surgery, at least 30% should remain from the liver after the part has been removed. With fibrosis, fatty hepatosis or cirrhosis (and they often accompany or precede liver cancer), this figure increases to 35-40%, otherwise the remaining liver with these pathologies will not be able to function adequately.
Localization of foci and their number. If metastases are multiple and “scattered” in several segments, then removing them is impractical: statistics show that the survival rate for such operations does not improve.
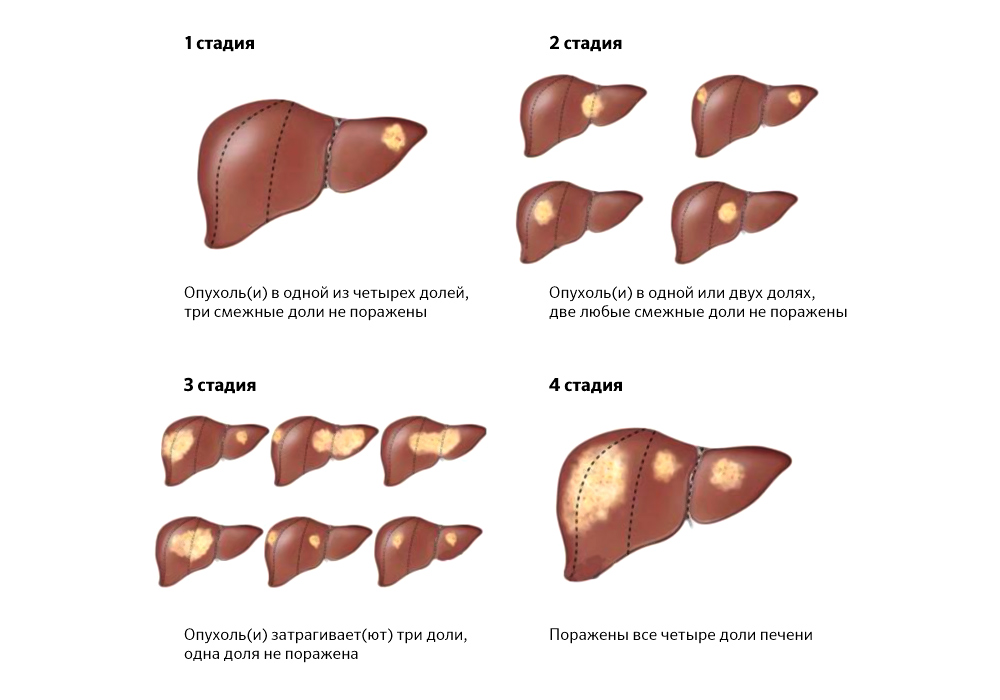
The prevalence of tumor foci sometimes makes surgical treatment impossible
Contraindications. These are the patient's health conditions that make the success of the intended operation statistically minimal.
1. Carcinomatosis of the peritoneum (carcinomatosis - less familiar to the ear, but medically more accurate term). Cancer cells from the primary focus with blood and lymph flow: they spread through the abdominal cavity and “germinate” in several organs at once.
2. Uncapable ascites - accumulation of a large amount of fluid in the abdominal cavity. In addition to the fact that it creates difficulties in the operation, ascites acts as a factor that provokes the spread of metastases. If it cannot be controlled, then it is highly likely that metastases recur rapidly.
3. Mechanical jaundice. The tumor site, squeezing the bile ducts, violates the outflow of bile and provokes the flow of bilirubin (a breakdown product of hemoglobin) into the blood. While accumulating, it stains the sclera (the whites of the eyes), the patient's skin and mucous membranes in yellow. This is dangerous: bilirubin is toxic and makes the patient's condition worse.
However, even for such patients who do not have surgery, there are treatments.
In cases where the patient is faced with the inability to remove the tumor in the liver by classical surgery, there is interventional oncology and endovascular (“intravascular”) surgery.
Hepatologists in Medicine 24/7 actively use them to improve survival rates. Like classical surgeries, these methods also have limitations, but thanks to them, many of our patients with unresectable liver tumors received a second chance to prolong life.
Chemoembolization of the vessels feeding the tumor is the main method of endovascular treatment of liver cancer. A thin catheter inserted through the femoral artery moves directly into the vessel supplying the tumor tissue and supplies the preparation containing microcapsules from a special medical plastic. They mechanically block the bloodstream, depriving the tumor cells of food, and secrete a drug against tumor growth, and directly into the lesion and in high concentration.
This method is able to reduce the tumor volume in the liver, and, therefore, in some cases - to make possible one of the options for surgical resection.
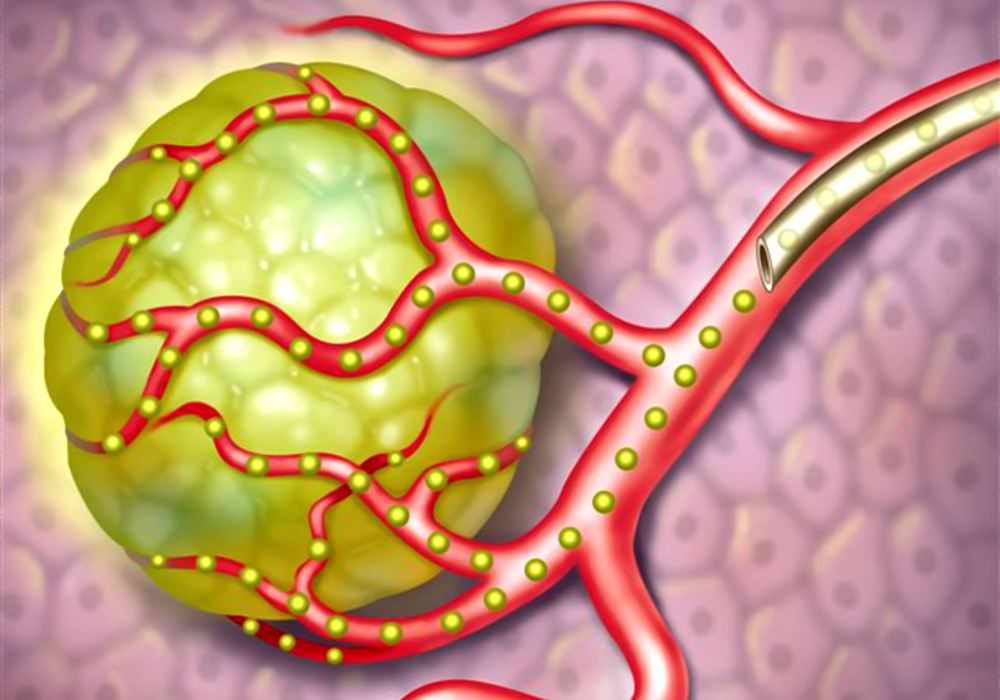
The scheme of the introduction of embolus (microcapsules) through the catheter directly to the tumor
Radiofrequency ablation of the tumor. Through a puncture in the skin, a thin electrode is supplied directly to the tumor center, at the end of which a radio frequency pulse creates a high temperature. And the surgeon purposefully “burns out” the neoplasm.
Stenting. Installing a stent (dilator) into a tumor-squeezed bile duct or vessel helps to overcome, for example, obstructive jaundice, to establish blood flow and outflow of bile — that is, remove one of the main contraindications for surgery.
These are the most popular methods in our clinic. In other cases, we use both cryodestruction (destruction of the tumor by low temperatures), and hyperthermic chemotherapy with HIPEC (against carcinoma of the peritoneum), and other suitable methods.
“The lack of competent surgeons is the most obvious difficulty faced by patients,” says Anton Alexandrovich Ivanov. - I have worked for 19 years both in state and private medicine, and everywhere there are enthusiastic doctors who do not have enough experience who say: “Let's cut it out now!”, Take the patient to the operating table, but do not perform the operation, what was needed, for example. Unfortunately, the prognosis for these patients does not improve after surgery. "
There are doctors who honestly admit that he does not do such operations, and sends the patient to large centers, to the capital cities. On the one hand, it is safer than a dropout surgeon, on the other hand, it is extremely difficult for such a patient to get free treatment. Even in the CHI system, surgery on the liver is not included in the standard of medical care. This is a high-tech surgical intervention performed according to quotas.
In any case, the patient must remember, no matter how frightening the verdict may be, it is necessary to get a second opinion: this is true not only in therapy, clinical oncology, but also in surgery.
In our Medicine 24/7, surgeons and hepatologists, despite their impressive experience, are sure to discuss each operation on the liver collectively in order to make the most balanced decision.
Price. For those who are not lucky enough to get a quota for free surgery, surgical treatment of liver tumors costs serious money. Within our private hospital, for example, resection itself, plus stay in the clinic, pre- and postoperative studies, reanimation - cost about 700,000 r.
Abroad, despite the fact that the same technologies are used and the same risks are present, liver surgery for metastatic lesions costs 6 times more expensive: from 60,000 euros.
Difficulties with transplantation. For each patient with unresectable tumors and the presence of contraindications to other interventions, ideally, there should always be one last chance: a liver transplant. But in Russia, transplantology is still lagging behind world experience.
In many ways - due to administrative problems. Legislation and licensing for transplantation of donor organs are not fully regulated; a large waiting list, and the lists of people in need of transplantation are not combined by region. In the EU, for example, the control system of donor organs is centralized: a suitable liver, which appeared in one of the countries, can be promptly brought to another country, where it is urgently needed.
In addition, the problem is in the public consciousness. In Western Europe or the United States, the consent of, say, nieces to give part of the liver to a transplant to an uncle is a fairly common subject. Our relatives refuse to become donors. Not all people know how successfully the liver recovers from which a part was taken away, but not all surgeons are ready to risk two lives, and not one.
Hope for bioengineering development: judging by the current work in this direction, in 20 years scientists will learn to “grow” an artificial liver in the right quantities. We sincerely hope to catch this moment.
In the meantime, bright minds of researchers come up with how to solve the problem of lack of donor material, the golden hands of our surgeons gain new experience.
The ALPPS technique (Eng. Associated Liver Partition and Portal vein ligation for Staged hepatectomy), described and tested by German surgeons in 2012, expands the possibilities for the surgical treatment of liver tumors previously considered unresectable .
The meaning of this two staged operation is not to remove the part of the liver affected by the tumor right away, but to separate it from healthy tissue, separate their blood flow and, as it were, make the patient two autonomous livers. After waiting 6-8 days until the remaining “piece” of healthy tissue grows to a size sufficient to perform its functions, and remove the metastases of the affected part in full.
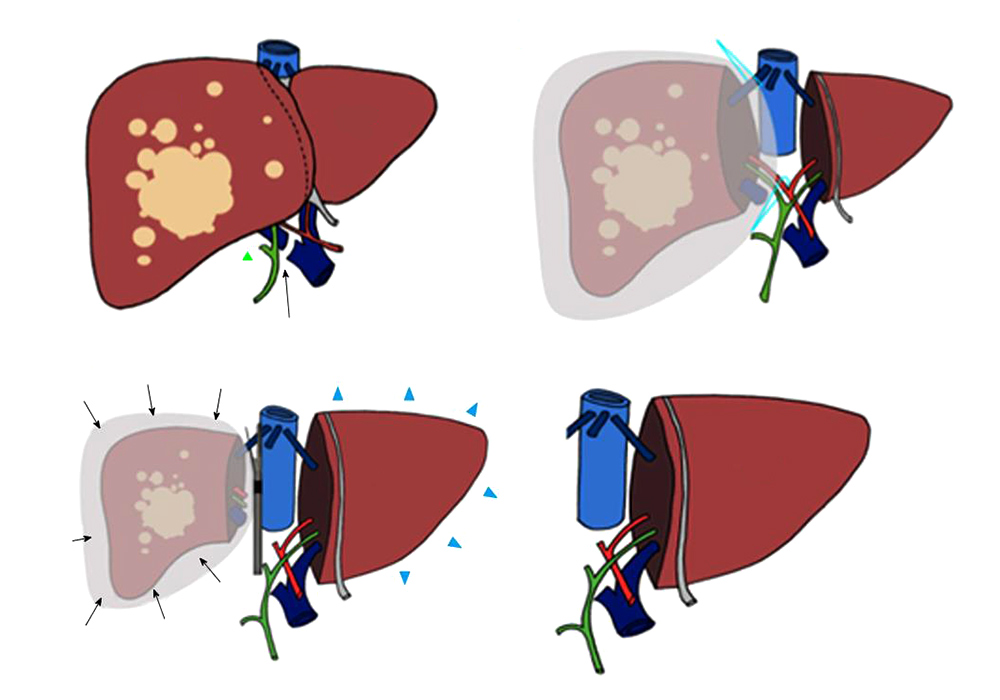
In a week, the left lobe of the liver grows to a size that allows it to work normally.
In Russia, ALPPS is not widely used yet, but the experience that our domestic colleagues already have shows as successful results as foreign surgeons.
The development of endoscopic surgery. Technical equipment is still developing rapidly. Now we can, using thin flexible microtools inserted into two skin punctures, cure a person, remove an entire organ, etc. Surgeons can perform very complex manipulations that were not possible 20-30 years ago. The quality of images from microscopic cameras during such operations is improved every year.
The main thing is that you need enough motivation and desire from doctors to learn and master these technologies. And of course, serious money is needed to purchase complex equipment and to train doctors. Both of these factors can rarely unite in a medical institution, even if it is an advanced scientific institute. And among private clinics, we are the only ones who perform a central resection of the liver.
The obvious answer: "Do not abuse alcohol." Permanent alcohol intoxication leads to hepatosis and cirrhosis of the liver: the hepatocytes die, and the voids in their place are replaced by scar connective tissue. Over time, this can lead to liver failure, as well as liver cancer.
About 5% of hepatocellular carcinomas are associated with aflatoxin, an extremely toxic substance that is produced by fungi that parasitize peanuts, sesame, sunflower seeds, corn, rice and other crops. Residents of civilized countries face it infrequently, but, nevertheless, it is very dangerous if you eat foods contaminated with such a fungus: the poison irreversibly damages the liver cells.
However, the most significant risk factor, according to statistics, more dangerous than alcohol, today is infection with viral hepatitis. Half a century ago, this was a problem in Asia and Africa, and today the incidence of hepatitis B and C in Europe, including in Russia, leads to an increase in the appearance of primary liver cancer. And it happens that hepatitis does not show symptoms, and people may not know for a long time that they are carriers of the virus.
Therefore, it is not necessary to neglect hepatitis B vaccinations and be checked annually for the presence of hepatitis C - vaccines have not yet been invented from it.
Regularly checked is the fundamental basis for the success of prevention, or at least early diagnosis (and therefore effective treatment).
“The sooner a tumor is detected, the more chances the patient has for successful radical treatment, surgically,” recalls Dr. Ivanov. - Therefore, every surgeon in Medicine24 / 7 will tell you: the key to success is a follow-up. It is still possible to pass through the MLA. But since the obligatory form of it no longer exists, it is better for you to take care of your health voluntarily: do an ultrasound, give the tumor markers adequate for your age, find out the family history. ”
And choose nuts more carefully. Just in case.
A radical method is one that eliminates the main problem and the cause of all other severe symptoms: a malignant neoplasm.
“Medicine 24/7” , first of all, is a surgical hospital with a serious load: among private clinics in Moscow, ours is in the first place for the consumption of blood and blood components that are necessary for operations.
Liver operations are not the most important and popular direction of the clinic. However, the fact that in our hospital, in principle, such manipulations are done, rather than sending patients somewhere else, is a marker and an indicator of the highest qualification of the surgeon’s team.
')
Operations on the liver are equivalent to operations on the brain and open heart. As a rule, this is the seventh complexity category out of 7.
At the same time, successful surgical treatment of malignant neoplasms in the liver makes it possible to count on the patient's life extension: five-year survival of 40-50% in primary liver cancer or single metastases is a good result.
We often receive patients who were not operated on at other clinics for some official reason. But people want to take a second chance, and we give it to them.
In this article we will try to explain why the liver so often requires attention in the treatment of cancer, why not every surgeon risks operating on it, and whether there are alternatives to the scalpel.
The venue: why cancer often affects the liver
The liver is an amazingly multi-tasking organ . The work can be divided into 3 directions.
1. Depositing. In the liver, the body stores many of the necessary things: energy reserves in the form of glycogen; some vitamins (A, D, B12, K, PP); trace elements (the main of which is iron).
Also here is a very significant amount of blood. If an unforeseen hole is formed in the body as a result of the injury, then this blood reserve will be urgently thrown into the main bloodstream and will compensate for blood loss for a while.
2. Synthesis. This organ is the “factory” of important hormones and enzymes. Many plasma proteins, including those by which blood coagulates when needed, but does not stick together in blood clots in ordinary life - are formed here. But most importantly, the liver produces bile, a component of healthy digestion.
3. detox. The liver is unique in that it is able to neutralize poisons, toxins, allergens and other dangerous substances that have entered the body from the outside, as well as originated as a product of our metabolism.
All these important functions of the liver are provided by its special blood supply system.
About 1.5 liters of blood pass through the liver in a minute. About a quarter of this volume enters the hepatic artery, and the remaining 75% through the portal vein from the intestine.
There are sinusoids inside the liver - special capillaries in which arterial blood is mixed with venous blood and this mixture is already “filtered” by hepatocytes (cells of the liver tissue): useful and nutrients are stored, toxins are neutralized as a result of complex chemical reactions. Then the blood, which has passed all the stages of "treatment", enters the hepatic vein and returns to the heart.
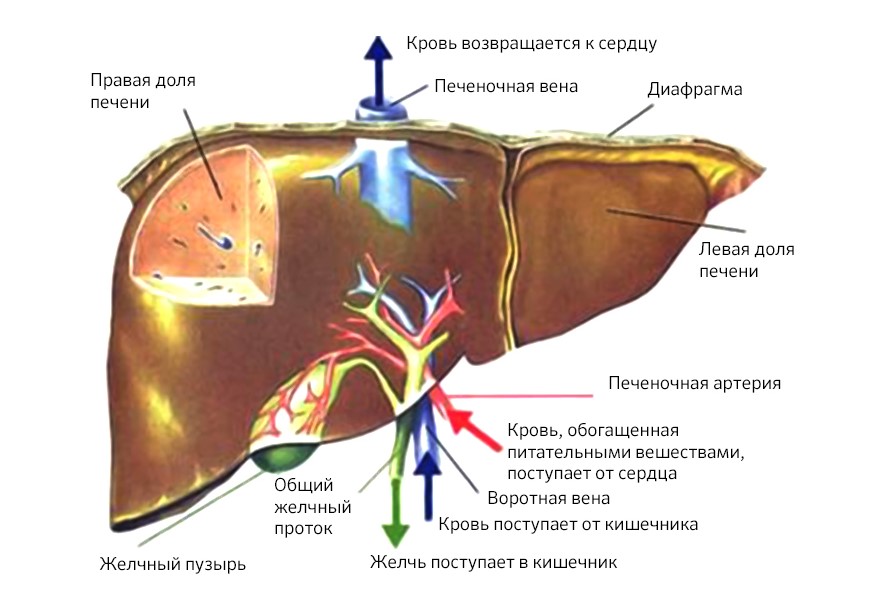
Circulation of blood in the liver
But this remarkable system, which allows the liver to filter 2,000 liters of blood per day, also contributes to the spread of cancer cells. They are carried through the body through the bloodstream, and the liver, which transmits and retains all that is superfluous, thus becomes a target for metastasis.
Liver tumors: hard to find, easy to start, sometimes impossible to cut
According to statistics, the primary liver tumor - hepatocellular carcinoma - is less common than metastases in this organ from other malignant neoplasms. The total number of patients with metastases in the liver in Russia is more than 100,000 - many times more than patients with primary tumors of the liver and intrahepatic bile ducts (less than 15,000).
But almost all malignant neoplasms metastasize to the liver. Colon cancer (colorectal cancer) does this in 50% of cases. In 30% of cases, metastatic lesions occur in melanoma and breast cancer.
Our leading oncologist surgeon in this field, Anton Aleksandrovich Ivanov, gives one of the most interesting examples in his practice.
“A patient with metastatic breast cancer in the liver. Usually such cases are not accepted to operate at all. But during the examination we found out that the liver is the only organ that has met metastasis. It was a rare success, and the surgeons made a collegial decision: to operate.
And when, in preparation for the operation, a biopsy of metastases was done, it turned out that cancer cells in the liver had mutated, and the initial HER2-negative status of the tumor changed, became HER2-positive, 3+. This means that the disease is sensitive to Herceptin, an effective remedy against this type of cancer. The patient was removed metastases, resected half of the liver. More than 10 years have passed, she receives the drug and is still alive. When she comes to the surveys, she complains not so much about her state of health, but rather of hooligans and grandchildren. ”
Unfortunately, both liver cancer and metastases in it are often diagnosed in an already neglected state.
Silently: why tumors in the liver are discovered too late
The reasons for this situation are the reverse side of the "superpowers" of the body. The liver has a huge margin of safety: to cope with its duties, it is enough for 15-20% of a healthy parenchyma (liver tissue).
“Tumors themselves do not hurt, but simply use the healthy tissue resource. So it turns out that a liver damaged by a tumor may not give signals at all until more than half of the organ is affected by the disease - and this is stage III-IV: 58% of primary liver tumors are detected in Russia in a state of neglected process, ”explains Anton Alexandrovich .
At the same time, ultrasound and even CT can skip a node in the liver, if it is still very small, and not in 100% of cases such studies make it clear the exact size, shape and nature of the focus.
This diagnostic complexity can be overcome: use of contrast media for hepatotropic (ie, targeting the liver) MRI. Only three of them, in Russia since 2007, one has been allowed and recommended for use: Primovist. It is able to accumulate in hepatocytes, but malignant tumors do not “absorb” it, due to this they become most clearly visible in the pictures.
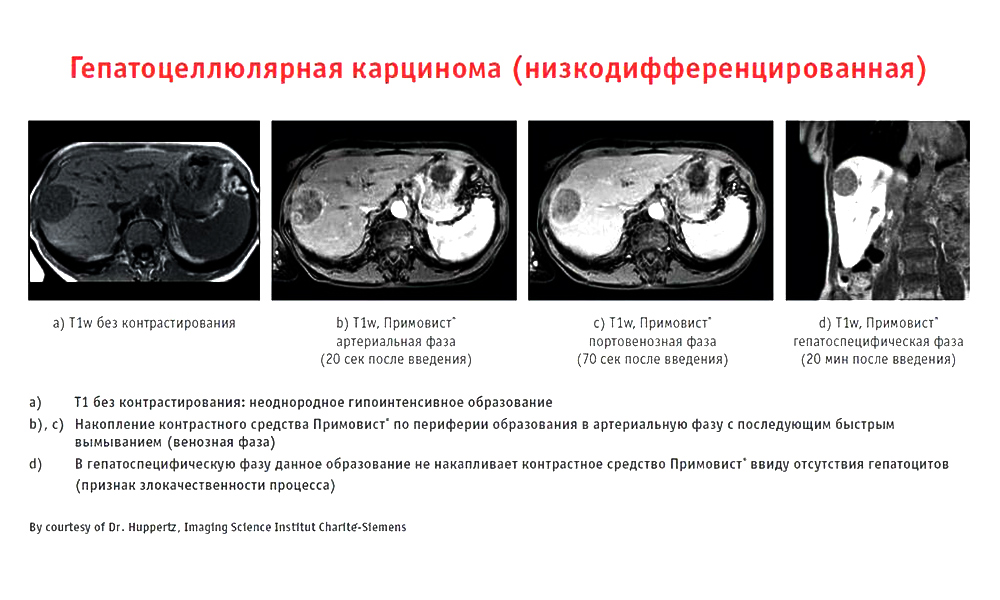
An example of the work of the contrast drug Primovist
Today, this drug is the gold standard for MRI diagnosis of liver tumors, the hepatologists in Medicine 24/7, use it without fail, which ensures an adequate level of accuracy.
But, unfortunately, in many regions the situation is more difficult: finding there clinics that know and use Primovist is still difficult, like 10 years ago.
Why not any surgeon can do surgery on the liver
Even finding a tumor in the liver, not every doctor will be able to remove it: it is more difficult for a surgeon to work in the hepatopancreatobiliary zone than read the word “hepatopancreatobiliary” the first time.
This zone includes the liver (Greek hepar), pancreas (lat. Pancreas), gall bladder (lat. Vesica biliaris) and bile ducts. All these organs are closely related anatomically and functionally.
Most interventions in other areas of surgery take place at one small specific location, and if we are talking about resection (removal of a part) of the liver, then the amount of work is great, even with one or two segments affected.
It is difficult, firstly, technically.
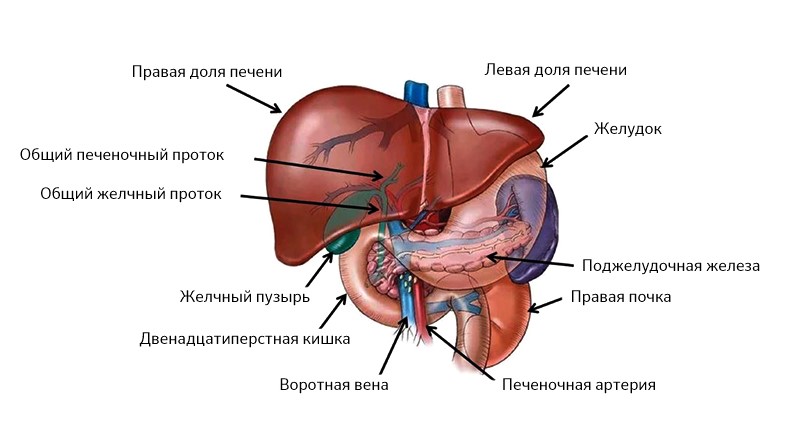
The liver is on the right side, the pancreas is on the left, all their ducts are combined into one and out into the duodenum
The liver is very complex, it consists of segments and lobes, between which there are ligaments, all of them literally enmeshed and penetrated by the veins, arteries and bile ducts.
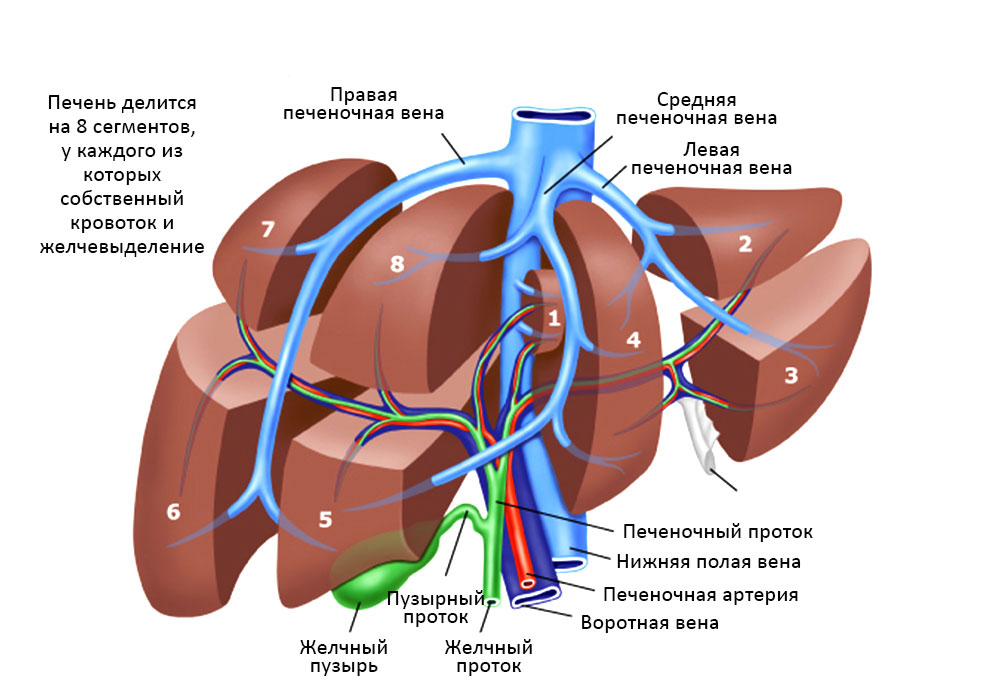
The relationship of the segments of the liver, bile ducts and blood vessels
There is a risk that a large vascular bundle is located in this area, everything happens very close to the inferior vena cava, hepatic artery: these are large great vessels. The liver itself is bleeding badly. Accordingly, there is a danger of serious blood loss, the operation should be as fast as possible and extremely accurate at the same time.
Such an intervention should be performed by a person with extensive experience in conducting these operations, and the number of such specialists goes to one. In Medicine 24/7, there are two of them at once, and patients often come to them in the direction from colleagues from other (highly respected) medical institutions, where, nevertheless, there are no specialists with sufficient skills.
How the operation goes: risk control and online decision making
Both the doctor and the patient are thoroughly prepared for liver surgery so that everything goes as predictably as possible. Anton Aleksandrovich Ivanov explained in detail how an oncologist and his team prepare for a liver surgery, and that they are trying to envisage everything.
“In order to accurately determine the scope and method of intervention, conduct all the necessary research. The area of operation is visualized with maximum accuracy. The results of multiple tests are taken into account. For example, in certain infectious diseases or a decrease in the number of platelets in the blood, the doctor will first select a therapy to restore normal parameters and only then prescribe an operation.
Immediately at the time of the intervention in the operating room, in addition to the doctor, there is a whole team of specialists monitoring the patient’s vital activities: anesthesiologists, resuscitators, transfusiologists, and an operating sister. Of course, today even the doctor does not remove the tooth alone, but liver operations collect the largest brigade in the operating room.
It is necessary to ensure the supply of blood components - erythrocyte mass, plasma, so that at any time with large blood loss it was possible to compensate for them. In our practice, we use a special device, Cell Saver, which immediately separates (separates) red blood cells from the patient’s lost blood and returns them back to its bloodstream. "Own" is always more favorable than "canned" donor erythrocytes, even suitable for the blood group. "
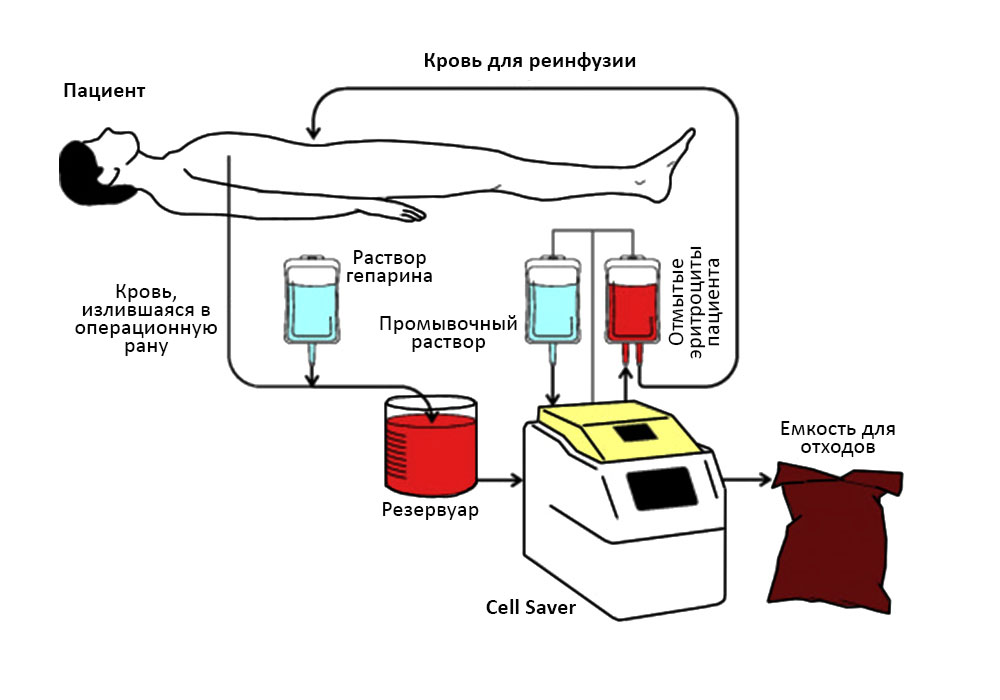
The patient’s blood enters the Cell Saver apparatus and he returns the red blood cells to the patient.
Quite regularly, surgeries are simultaneous (simultaneous): liver resection takes place simultaneously with other interventions. Removed and the primary focus, for example, in the colon, and metastasis in the liver.
However, even with maximum predictability and complete control of the process, surgeons happen to deviate from the intended plan.
For example, during surgery for a primary tumor of the stomach, an occasional find may occur: a small single metastasis in the liver. In this case, surgeons can invite colleagues, specialists in operations on the liver, so that they spend their stage: removal of a part of the liver.
Joint operations are good because the patient is subjected to anesthesia and the difficulties of the recovery period only once.
By the time the operation takes from 1.5 hours (with resection of a single metastasis) to 10-12. “In my practice, the longest operation with simultaneous removal of the primary focus in the intestine and liver metastases lasted 15 hours,” recalls Dr. Ivanov, “but this case is rather exceptional.”
Not all tumors are equally operable.
Size matters. If the tumor is large, it managed to “eat” too much healthy tissue, then removing it may be meaningless. In order for the patient to have a guaranteed surgery, at least 30% should remain from the liver after the part has been removed. With fibrosis, fatty hepatosis or cirrhosis (and they often accompany or precede liver cancer), this figure increases to 35-40%, otherwise the remaining liver with these pathologies will not be able to function adequately.
Localization of foci and their number. If metastases are multiple and “scattered” in several segments, then removing them is impractical: statistics show that the survival rate for such operations does not improve.
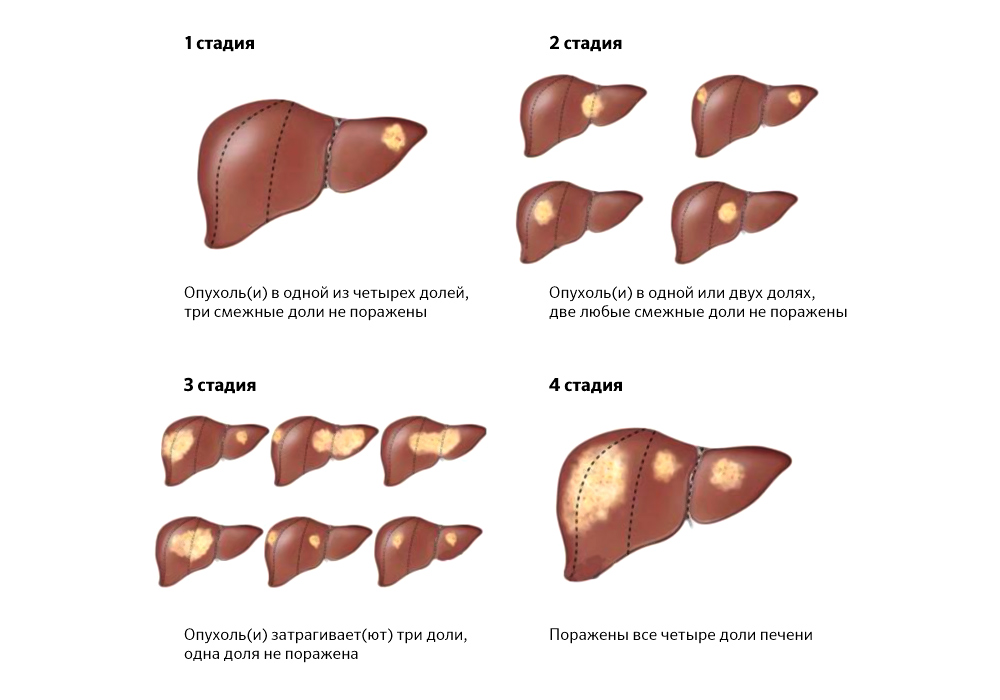
The prevalence of tumor foci sometimes makes surgical treatment impossible
Contraindications. These are the patient's health conditions that make the success of the intended operation statistically minimal.
1. Carcinomatosis of the peritoneum (carcinomatosis - less familiar to the ear, but medically more accurate term). Cancer cells from the primary focus with blood and lymph flow: they spread through the abdominal cavity and “germinate” in several organs at once.
2. Uncapable ascites - accumulation of a large amount of fluid in the abdominal cavity. In addition to the fact that it creates difficulties in the operation, ascites acts as a factor that provokes the spread of metastases. If it cannot be controlled, then it is highly likely that metastases recur rapidly.
3. Mechanical jaundice. The tumor site, squeezing the bile ducts, violates the outflow of bile and provokes the flow of bilirubin (a breakdown product of hemoglobin) into the blood. While accumulating, it stains the sclera (the whites of the eyes), the patient's skin and mucous membranes in yellow. This is dangerous: bilirubin is toxic and makes the patient's condition worse.
However, even for such patients who do not have surgery, there are treatments.
Alternatives to scalpel
In cases where the patient is faced with the inability to remove the tumor in the liver by classical surgery, there is interventional oncology and endovascular (“intravascular”) surgery.
Hepatologists in Medicine 24/7 actively use them to improve survival rates. Like classical surgeries, these methods also have limitations, but thanks to them, many of our patients with unresectable liver tumors received a second chance to prolong life.
Chemoembolization of the vessels feeding the tumor is the main method of endovascular treatment of liver cancer. A thin catheter inserted through the femoral artery moves directly into the vessel supplying the tumor tissue and supplies the preparation containing microcapsules from a special medical plastic. They mechanically block the bloodstream, depriving the tumor cells of food, and secrete a drug against tumor growth, and directly into the lesion and in high concentration.
This method is able to reduce the tumor volume in the liver, and, therefore, in some cases - to make possible one of the options for surgical resection.
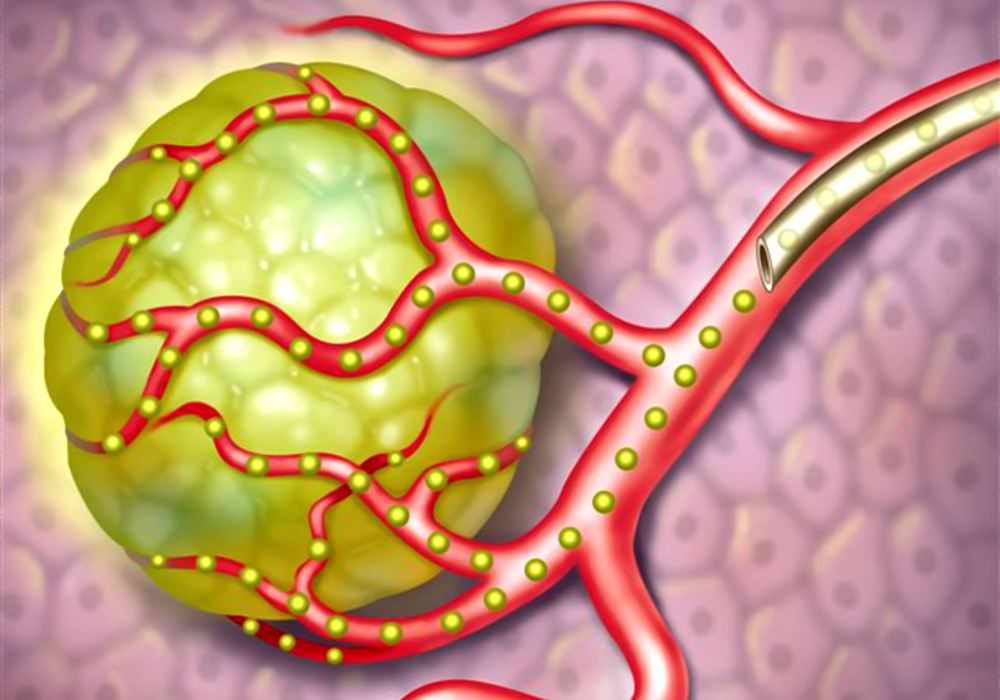
The scheme of the introduction of embolus (microcapsules) through the catheter directly to the tumor
Radiofrequency ablation of the tumor. Through a puncture in the skin, a thin electrode is supplied directly to the tumor center, at the end of which a radio frequency pulse creates a high temperature. And the surgeon purposefully “burns out” the neoplasm.
Stenting. Installing a stent (dilator) into a tumor-squeezed bile duct or vessel helps to overcome, for example, obstructive jaundice, to establish blood flow and outflow of bile — that is, remove one of the main contraindications for surgery.
These are the most popular methods in our clinic. In other cases, we use both cryodestruction (destruction of the tumor by low temperatures), and hyperthermic chemotherapy with HIPEC (against carcinoma of the peritoneum), and other suitable methods.
Problems and predictions in the surgical treatment of liver tumors
“The lack of competent surgeons is the most obvious difficulty faced by patients,” says Anton Alexandrovich Ivanov. - I have worked for 19 years both in state and private medicine, and everywhere there are enthusiastic doctors who do not have enough experience who say: “Let's cut it out now!”, Take the patient to the operating table, but do not perform the operation, what was needed, for example. Unfortunately, the prognosis for these patients does not improve after surgery. "
There are doctors who honestly admit that he does not do such operations, and sends the patient to large centers, to the capital cities. On the one hand, it is safer than a dropout surgeon, on the other hand, it is extremely difficult for such a patient to get free treatment. Even in the CHI system, surgery on the liver is not included in the standard of medical care. This is a high-tech surgical intervention performed according to quotas.
In any case, the patient must remember, no matter how frightening the verdict may be, it is necessary to get a second opinion: this is true not only in therapy, clinical oncology, but also in surgery.
In our Medicine 24/7, surgeons and hepatologists, despite their impressive experience, are sure to discuss each operation on the liver collectively in order to make the most balanced decision.
Price. For those who are not lucky enough to get a quota for free surgery, surgical treatment of liver tumors costs serious money. Within our private hospital, for example, resection itself, plus stay in the clinic, pre- and postoperative studies, reanimation - cost about 700,000 r.
Abroad, despite the fact that the same technologies are used and the same risks are present, liver surgery for metastatic lesions costs 6 times more expensive: from 60,000 euros.
Difficulties with transplantation. For each patient with unresectable tumors and the presence of contraindications to other interventions, ideally, there should always be one last chance: a liver transplant. But in Russia, transplantology is still lagging behind world experience.
In many ways - due to administrative problems. Legislation and licensing for transplantation of donor organs are not fully regulated; a large waiting list, and the lists of people in need of transplantation are not combined by region. In the EU, for example, the control system of donor organs is centralized: a suitable liver, which appeared in one of the countries, can be promptly brought to another country, where it is urgently needed.
In addition, the problem is in the public consciousness. In Western Europe or the United States, the consent of, say, nieces to give part of the liver to a transplant to an uncle is a fairly common subject. Our relatives refuse to become donors. Not all people know how successfully the liver recovers from which a part was taken away, but not all surgeons are ready to risk two lives, and not one.
Hope for bioengineering development: judging by the current work in this direction, in 20 years scientists will learn to “grow” an artificial liver in the right quantities. We sincerely hope to catch this moment.
In the meantime, bright minds of researchers come up with how to solve the problem of lack of donor material, the golden hands of our surgeons gain new experience.
The ALPPS technique (Eng. Associated Liver Partition and Portal vein ligation for Staged hepatectomy), described and tested by German surgeons in 2012, expands the possibilities for the surgical treatment of liver tumors previously considered unresectable .
The meaning of this two staged operation is not to remove the part of the liver affected by the tumor right away, but to separate it from healthy tissue, separate their blood flow and, as it were, make the patient two autonomous livers. After waiting 6-8 days until the remaining “piece” of healthy tissue grows to a size sufficient to perform its functions, and remove the metastases of the affected part in full.
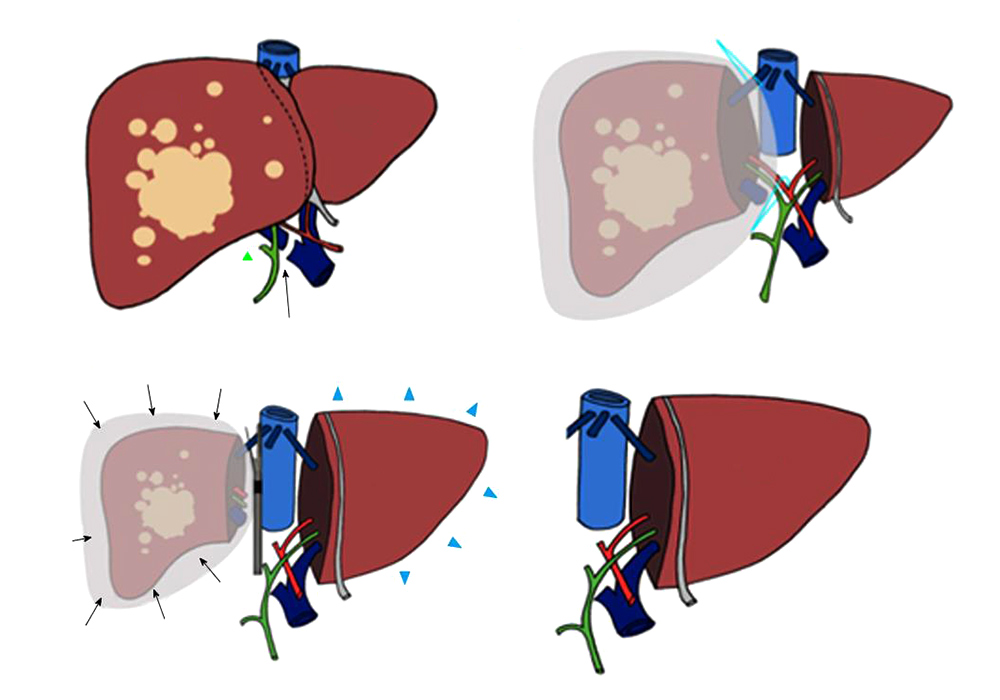
In a week, the left lobe of the liver grows to a size that allows it to work normally.
In Russia, ALPPS is not widely used yet, but the experience that our domestic colleagues already have shows as successful results as foreign surgeons.
The development of endoscopic surgery. Technical equipment is still developing rapidly. Now we can, using thin flexible microtools inserted into two skin punctures, cure a person, remove an entire organ, etc. Surgeons can perform very complex manipulations that were not possible 20-30 years ago. The quality of images from microscopic cameras during such operations is improved every year.
The main thing is that you need enough motivation and desire from doctors to learn and master these technologies. And of course, serious money is needed to purchase complex equipment and to train doctors. Both of these factors can rarely unite in a medical institution, even if it is an advanced scientific institute. And among private clinics, we are the only ones who perform a central resection of the liver.
How to save the liver
The obvious answer: "Do not abuse alcohol." Permanent alcohol intoxication leads to hepatosis and cirrhosis of the liver: the hepatocytes die, and the voids in their place are replaced by scar connective tissue. Over time, this can lead to liver failure, as well as liver cancer.
About 5% of hepatocellular carcinomas are associated with aflatoxin, an extremely toxic substance that is produced by fungi that parasitize peanuts, sesame, sunflower seeds, corn, rice and other crops. Residents of civilized countries face it infrequently, but, nevertheless, it is very dangerous if you eat foods contaminated with such a fungus: the poison irreversibly damages the liver cells.
However, the most significant risk factor, according to statistics, more dangerous than alcohol, today is infection with viral hepatitis. Half a century ago, this was a problem in Asia and Africa, and today the incidence of hepatitis B and C in Europe, including in Russia, leads to an increase in the appearance of primary liver cancer. And it happens that hepatitis does not show symptoms, and people may not know for a long time that they are carriers of the virus.
Therefore, it is not necessary to neglect hepatitis B vaccinations and be checked annually for the presence of hepatitis C - vaccines have not yet been invented from it.
Regularly checked is the fundamental basis for the success of prevention, or at least early diagnosis (and therefore effective treatment).
“The sooner a tumor is detected, the more chances the patient has for successful radical treatment, surgically,” recalls Dr. Ivanov. - Therefore, every surgeon in Medicine24 / 7 will tell you: the key to success is a follow-up. It is still possible to pass through the MLA. But since the obligatory form of it no longer exists, it is better for you to take care of your health voluntarily: do an ultrasound, give the tumor markers adequate for your age, find out the family history. ”
And choose nuts more carefully. Just in case.
Source: https://habr.com/ru/post/454886/
All Articles