Get up and go. Spinal surgery: when to do, what is dangerous
TOP3 myths about the patient's back, which prevent people from once and for all solve their problem.
The warmer, the more often patients with complaints of back pain come to us at Medicine 24/7 . Someone has already opened the summer season, and someone was in a hurry to pump up by the summer.
And every day we get such results of examinations of these people, that they absolutely clearly show spinal surgery. She quickly and permanently relieve them of pain, "lumbago", "jamming" in the lower back, numbness of the limbs and more severe problems.
')
But Russian patients and, even worse, doctors - are trying to the last to avoid spinal surgery. It is still widely regarded as dangerous. And for safe neurosurgery, it is customary to go except to Germany and pay around 30,000 euros. Patients who are not ready for such expenses are forced to relieve the symptoms of hernia and stenosis with drugs and physiotherapy. But these measures do not remove the problem, but only make it possible to live with it, experiencing constant inconvenience, limiting oneself in movements, choice of hobbies, work and even posture for sleeping.
Now “Medicine 24/7” is the first and so far the only clinic in the country that performs endoscopic treatment of stenoses and hernias using the Joimax minimally invasive spinal surgery technology. On the German equipment with the price per operation is 7 times lower than in Germany.
Every day we prescribe people who, after a spinal surgery, leave us the next day on their feet, return to life without anti-inflammatory ointments and painkillers.
But most of the patients still continue to be afraid of surgery. Fears, most often, are based on those very myths about the inevitable danger of operations and the "conspiracy of surgeons." But doctors have long known the origin of the horror stories - as always, this is a lack of reliable information.
So today we will tell you how modern spinal surgery is done, whether the risks are really great, and how to live so as not to get to the table with the surgeon.
Why back hurts and why you can not tolerate
Almost every person over 20 at least once had a back pain. What is the reason?
The musculoskeletal system of Homo sapiens is well suited for erect walking, and in some places it even stores nostalgic memories of aging (for example, the broadest back muscles, which are now needed only for climbers and bodybuilders).

The broadest muscles of the back. Before any bodybuilder gorilla far.
Our main support - the spine - is made so as to spring up and soften the "recoil" when walking, running and other fast sudden movements. This is due both to its ventral (forward) and dorsal (backward) bends, and due to elastic “spacers” between the vertebrae - the intervertebral discs.

The spinal column is springy as a kind of hybrid of spring and shock absorber.
But a comfortable civilized life began, by historical standards, just yesterday, and life did not prepare us for this. It is not stipulated by human biomechanics that the body will sit motionless in a car for 3 hours a day and at a computer for 8-10 hours. But it is worth while rejecting the spine from the vertical or changing its natural deflection (for example, slouching) - the pressure on the intervertebral discs grows many times.

The pressure on the intervertebral discs in different conditions, the standing position is taken as 100% and is 5 bar (compare: in the car tire - 2 bar)
Nature did not expect that it would become fashionable to carry weights three times a week in the gym for the sake of beauty.

The load on the lumbar spine when exercising with a weight - up to 730 kg
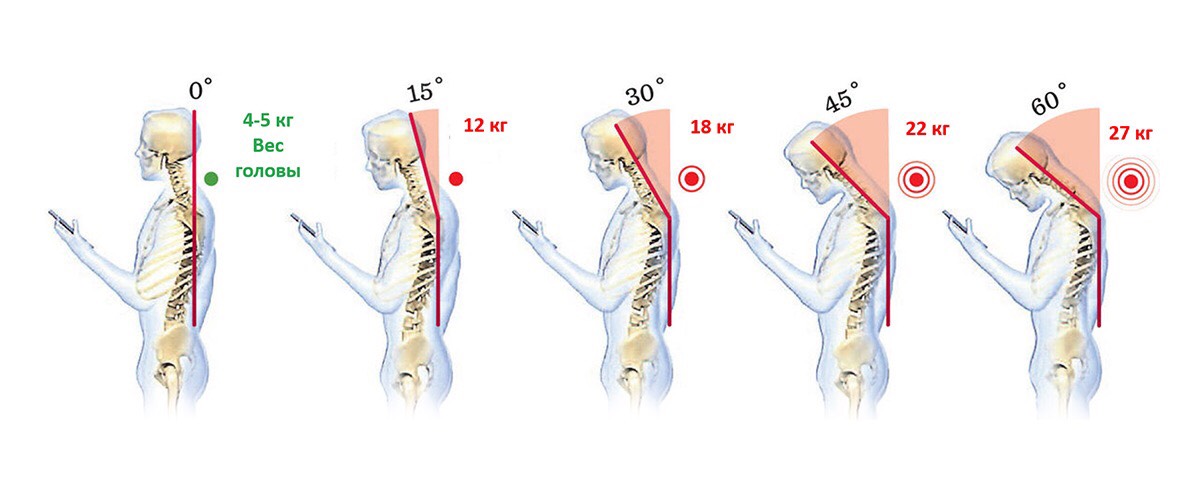
How many kilograms hang on your neck when you take out a smartphone?
The general conclusion is that the spine suffers for various reasons in almost all modern city dwellers. You or your acquaintances almost certainly have backache or neck pain, discomfort and numbness in the limbs, sharp headaches, tinnitus, and front sight.
But people are so accustomed to these symptoms in everyday life, that they simply adapt to them: they put pillows on them, turn over on the other side, or smear their backs with ointment from TV commercials.
Almost 90% of our patients, before coming with complaints to the clinic, engaged in self-treatment. Many have only exacerbated this problem. While a person lives with pain, changes, often irreversible, occur in his bone, cartilage, nervous tissue.
Pain - the first signal of such changes. Therefore, it can not be tolerated by anyone - it does not matter that you are still young and used to it, that you usually have “nothing serious”.
Going to a doctor in time and doing an MRI - this small effort can save you years of free movement and prevent really serious problems, even paralysis.
Hernia, protrusion, stenosis and other troubles
The most common cause of acute back pain, movement disorders and work of the limbs in patients of relatively young age (up to 50 years) is a herniated disc.
Here are healthy vertebrae and a disc in between.
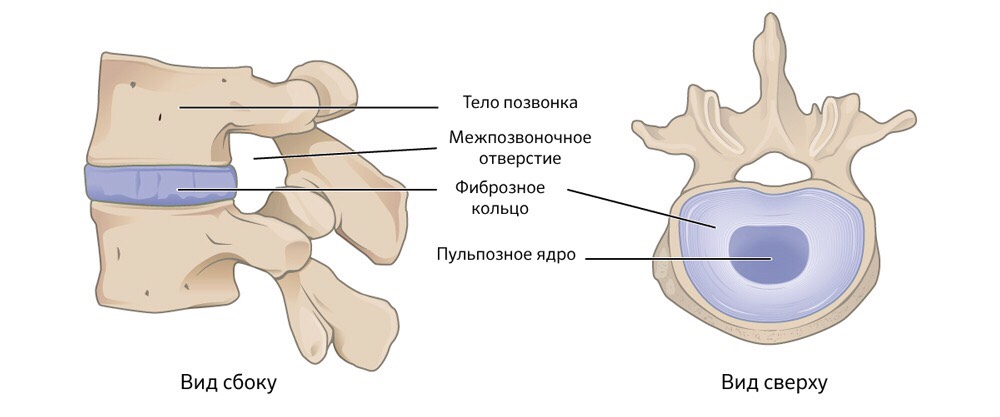
The structure and position of a healthy intervertebral disc
The disk consists of a dense fibrous fibrous ring, inside of which there is a gel-like structure - a pulp core. Top and bottom of the disc is covered with cartilage tissue.
Intervertebral discs do the work of shock absorbers when we move, sit for a long time, or stand. They prevent contact and abrasion of the vertebrae. If the intervertebral disc is subjected to strong pressure for too long and regularly, degenerative-dystrophic changes occur in it.
The fibrous ring is gradually deformed, becomes uneven thickness. And the pulpous core is still under stress. Where the thickness of the “crumpled” fibrous ring is minimal, the core pushes it outward, beyond the boundaries of the vertebral body. This protrusion in violation of the homogeneity of the fibrous ring is called protrusion.
It may not cause serious problems. If you take precautions, with protrusion, you can safely live a lifetime. But it is dangerous that the problems are already there, and without symptoms the person does not know about them and does not consider it necessary to protect the spine.
Then the protrusion increases with time. And where the fibrous ring is thin, it breaks there. The pulpous core is squeezed out. This is a hernia.
If it goes in the direction of the spinal canal, it squeezes the spinal cord or nerve roots passing there, causing great pain and disrupting nerve conduction.
Acute pain syndrome, immobilization (“wedged back”), disruption of the limbs, dizziness, and sometimes even temporary paralysis and dysfunction of some organs appear.

The development of the degenerative process in the intervertebral disc
Hernia can happen in both 20 and 70 years, but in old age (after 50 years) the cause of back and limb problems is often not a sharp, as in the case of hernia, but a gradual chronic process. Stenosis - narrowing of the spinal canal.
The reasons are common: age-related changes of intervertebral discs, their "wear". Consequently, destabilization of the vertebrae, reduction of the distance between them, overstrain of the facet joints. Plus a decrease in bone density and weakening of the muscles, making the vertebrae even worse withstand the load.
The body is trying to compensate for the instability of the spinal column, building up tight dense structures in "weak spots". Hypertrophy (enlargement) and ossification (ossification) of the yellow ligament, growth of the facet joints, formation of osteophytes (bone tissue growths) often develop. All these "additional fortifications" take place, narrowing the spinal canal.

The most likely causes of spinal stenosis
All this leads to pain syndromes, to neurogenic limp, etc.
How it is treated without surgery
If there is stenosis, protrusion or hernia, but there is no compression of the roots, impaired reflexes, movements and sensitivity, and there is only pain in the lumbar region, conservative treatment is prescribed. It includes three blocks - physiotherapy, physiotherapy exercises (LFK), and drug therapy.
Physiotherapy is a common name for a variety of therapeutic measures. These are methods of hardware exposure: tissue electrostimulation, magnetic therapy, electro- and phonophoresis; traction on a special rehabilitation simulator "Exarta"; soft manual techniques, massage.
Classes are added with an instructor LFK. He helps the patient to remove the musculo-tonic syndrome (prolonged spasms that damage the muscle fibers), teaches correct movements and exercises, monitors the correct technique of performance and the adequacy of the load, explains what cannot be done with this diagnosis.
Drug therapy is the third block. These are anti-inflammatory and painkillers that relieve muscular-tonic syndrome; vitamin therapy (milgamma, a complex of vitamins of group B); drugs that restore the conductivity of nerve fibers. These include tablets, injections, and topical ointments. Drug treatment has the main objectives: relieve spasm, remove pain, reduce swelling and improve blood circulation.
The main problem - conservative treatment removes the symptoms, but does not affect their source, the pathology itself. The main "mechanical" cause of problems does not go anywhere, a hernia or stenosis cannot "resolve" by themselves.
Physiotherapy can last for years. The patient becomes easier at the time. Then the aggravation returns, again you need to undergo a course of therapy. Conservative treatment requires an average of 1-2 times a year to invest in the back from 30,000 to 120,000 rubles. for medications and physiotherapy, so that you do not have to endure the pain and not get worse.
But conservative treatment is historically considered to be less risky than surgery aimed at eliminating the main problem. About 70% of cases of protrusions, hernias and stenoses are limited in testimony to conservative treatment today. So horror films about evil surgeons who never agree to send a patient to a pharmacy and to a massage, but only dragged into the operating room - this is nothing more than a folk exaggeration.
Spinal surgery: danger or necessity?
However, a problem arises when there are indications for surgery, but patients spend resources on ineffective treatment, and don’t go for surgery - because neither they nor, unfortunately, their doctor simply knows that operations can be safe. .
In the recent past, the only way to get to the spine was an open surgery. Such interventions are indeed associated with serious complications.
How to conduct open surgery
An incision is made at the level of the hernia, not less than 3-4 cm (up to 8) in length, the skin is dissected, the muscles are separated, access to the spine is released. Then a yellow ligament opens up: for this purpose, the pliers remove the bows of the underlying and overlying vertebra so that you can see the structures in the spinal canal. With a special hook, the nerve root is set aside, a hernia is cut.

The schematic image of the removal of the hernia with open surgery
If the operation is performed for stenosis, everything goes in a similar way, but a part of the ligaments and bone tissue of the vertebra is removed, sufficient to achieve decompression of the strangulated nerve roots - in other words, to give them additional space.

Open surgery for spinal stenosis
The main difficulty of the majority of open surgeries with resection of bone structures - after removal of parts of the vertebrae, destabilization of the spinal column occurs: the overlying vertebrae have nothing more to rely on. To correct the situation, pedicle clamps are inserted - from 4 to 6 screws are screwed in to keep the spine in the right condition. Implantation of any "iron" looks cool only in comics, but in life it is a risky event.

Titanium screws to ensure the stability of the damaged spine
Full recovery after an open operation takes 4-6 months, the patient cannot sit for a long time and moves with difficulty, needs rehabilitation with the help of physiotherapy, massage, and medications.
Consider possible complications during open surgery.
Irreversible damage to the nerve roots. To open the yellow ligament or resect part of the overlying / underlying vertebra, you need to forcefully press on the nippers. And even an experienced surgeon will not give a 100% guarantee that at this moment an instrument or bone fragment will not damage the nerve.
Durotomy. Damage to the dura mater around the spinal cord. Not a rare event during manipulations on the spine, which can lead to damage to the nervous tissue and the outflow of cerebrospinal fluid - liquorrhea. And this is again the compression of the roots and spinal cord, pain and movement disorders, the risk of developing meningitis.
The formation of scars and adhesions. Contact of nerve roots with air provokes excessive scar formation. And even if the operation was successful, the replacement of the nervous tissue in the root with the connective tissue of the scar eliminates the results of the operation and leads to a re-deterioration of the patient's condition.
Despite the complexity and risks of open operations, they are still regularly done around the world. The main reason for such a commitment to tradition is open operations that are undemanding to the technological equipment of the hospital. They do not need to buy expensive equipment and upgrade the skills of surgeons and medical staff.
Endoscopic operations require the purchase of new technology, training of doctors - and this is a serious expense.
An experienced neurosurgeon will understand the technology of endoscopic interventions for a week, but for this he needs to go to training with German or American colleagues, and then himself conduct at least 30 operations on Joimax or similar equipment. In Russia, such a technique is almost impossible to find: it costs 20,000,000 rubles - an adequate price for complex high-tech technologists, but unrealistically huge amounts of money for domestic hospitals.
Therefore, patients with hernia, stenosis, and radicular symptoms: pain, impaired reflexes, and movements — who have not received adequate help for years, come to Medicine 24/7 regularly. Although our neurosurgeons could have relieved them of the problem for a long time, it was less traumatic, quickly and definitively.
How to operate the spine without incisions?
Many modern operations become closed, endoscopic: special thin tubes-manipulators with micro tools and video cameras at the ends are inserted through the punctures in the skin - the doctor sees everything he does without risking damage to bone structures, nerve tissues or muscles. For neurosurgery with its high risks, this is especially useful, and here minimally invasive endoscopic access becomes the quality standard.
True, this requires sophisticated modern equipment. It is produced by only a few companies, mostly German, and even they are not equally good. Neurosurgeons of our clinic, while they were going to study in Germany, tried all the available technology options, and stopped at Joimax - this equipment allows you to work on all spinal sections and solve all problems.
The main advantage of endoscopic operations is minimal trauma. Access to the affected area occurs through natural anatomical windows between the bone structures of the spinal column: intralaminar (between the vertebral arches) or transforaminally (through the intervertebral foramen). In this case, the doctor does not violate the biomechanics of the spine, does not open the spinal canal, does not remove part of the vertebra to get to the place of nerve compression.

Neurosurgeon does not look at the patient during endoscopic surgery.

He looks at the monitor, where he sees everything that happens from the inside.
An MRI / CT scan is performed before the operation. Sometimes functional images are assigned to see if there is no fidez (displacement of the vertebral bodies relative to each other) but, as a rule, MRI and CT are sufficiently informative. By the time of surgery, the doctor understands exactly what will happen and how.
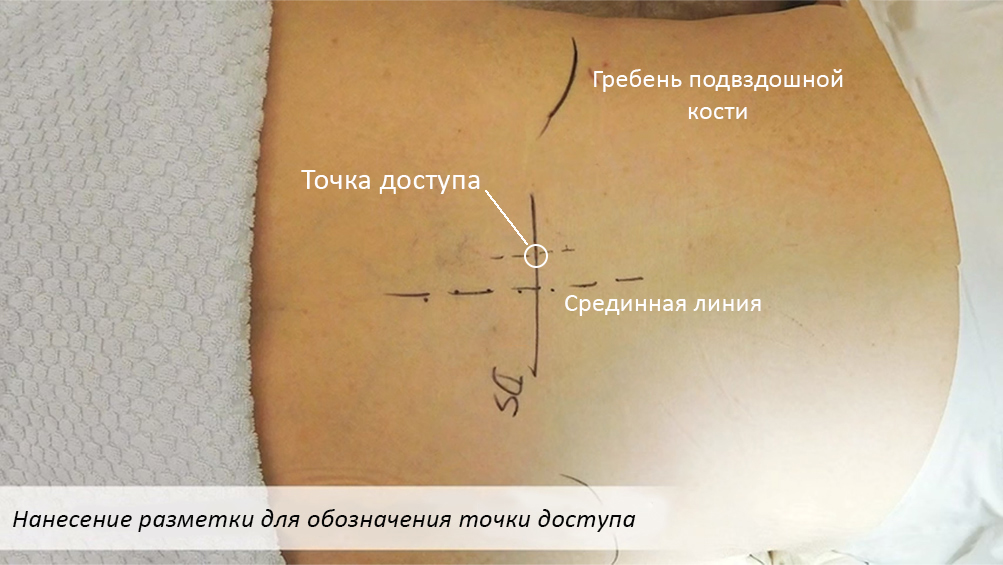
Reconnaissance on the ground - the access point is clear to the millimeter
A micro-cut is made at the exact location. Special tubes are introduced into it, gradually gently widening the hole and serving as guides for endoscopic instruments. The accuracy of administration at this stage is constantly monitored by X-rays. The working tube remains in the patient until the end of the operation.
And then an endoscope is inserted into the tube: a special instrument, which, in fact, is also a hollow tube. At the end of the endoscope is a video camera and a light source, and a channel for all other instruments passes through it.The endoscope is also inserted once at the beginning of the operation, and other instruments are delivered to the scene of action through it as needed.

Endoscope and instrument inserted through it.
A cable is connected to the endoscope through which the image from the endoscope camera is transmitted to the monitors in the operating room. The neurosurgeon sees all the capillaries, vessels, nerves, ligaments, bones with an increase of more than 50 times (compare: an ordinary operating microscope increases 20-30 times).
Through the endoscope, one can literally with jeweler precision remove excess tissue that causes a narrowing of the lumen of the spinal canal and compression of the nervous structure. To perform a resection of soft and hard tissues, grind off “extra” bone structures with a diamond cutter, rinse the operated area — moreover, the cut-off parts of the tissues, bone dust and fluid are removed through the same endoscope.

The process of resection of a hernia with special forceps inserted through an endoscope. In the upper right corner shows how this moment looks on the x-ray.
The whole operation takes an average of an hour. The longest case in the practice of our clinic is 4 hours, removal of complex stenosis in the lumbar region. A large number of growths took time to carefully remove them: the grinding of bone tissue with a diamond cutter is a delicate and gradual process.
But the main thing, of course, is not that it is more convenient, faster and easier for a neurosurgeon to work using Joimax technologies. The benefits are in patients. Treatment of stenosis or hernia with minimally invasive endoscopic surgery is devoid of complications, risks, and simply the inconvenience inherent in open surgery.
Blood loss is minimal. With an open operation, the muscles are opened, the bone is bitten off, the bleeding will necessarily be (yes, the bones also bleed). When working with a high-speed cutter, there is no blood. The cutter turns the bone into dust, and the damage to the vessels is simply "sealed."
Visual inspection reduces the risk of accidental damage.If, for example, inadvertent damage to the membrane occurs around the spinal cord, the doctor will see it immediately and eliminate it, avoiding complications such as liquorrhea (the expiration of the CSF).
The absence of contact with air eliminates the pathological scarring of the nervous tissue and the formation of adhesions.
Accessibility for patients with diabetes, obesity, diseases of the cardiovascular system. Open operations are contraindicated in them, since will cause serious complications. With endoscopic complications will not. In Medicine 24/7, such patients receive help when conservative treatment has completely stopped working. In other clinics, these people, most likely, have already been refused. But Joimax technology is safe even for them, and, most importantly, effective. People stop to suffer.
Rapid rehabilitation. During endoscopic spinal surgery there are no massive operative injuries, after the operation there are no drains left, metal implants - only a 1.5 cm suture. The patient gets up after 12 hours, and within a few days returns to the usual life.
Maybe to massage, and not to operate?
It is logical that people are still afraid of surgery, even minimally invasive, but sometimes they choose on their own much more dangerous methods of treatment, mistakenly considering them a soft alternative.
Private “Healthy Back Centers”, manual and osteopaths today are fashionable and in demand, but may be more risky than an operation.
Often they save time on diagnosis. Everyone is offered the same thing, regardless of diagnoses, the level and nature of pain syndromes. Bad manual therapists treat patients without an MRI or at least x-rays.
Remember, a “hands-on” treatment can aggravate the problem. Patients regularly come with exacerbations and deterioration of the situation after a visit to a “private man” therapist or to a dubious “spinal health clinic”. When, for example, a person with a hernia of the cervical region (an absolute contraindication for massage) begins to "crack the vertebrae," and he comes to us by ambulance.
Manual therapy is great, but careful, only as directed by a doctor, only after an accurate diagnosis. If the "doctor" puts you on a massage table, not interested in the history, it is better to find another.
Summary
Even 50 years ago, people were afraid of dentists, and they could be understood, but now the treatment of a tooth does not cause pain and takes minimal time at any clinic. With spinal surgery the same situation.
For Medicine 24/7, safe, accurate and efficient endoscopic neurosurgery has been a familiar standard for several years, but patients and even many of our industry colleagues simply do not know that safe radical treatment is available in Russia. And they continue to consider the danger of spinal surgery in general, although the risks of endoscopic intervention cannot be compared with the risks of open operations.
Often the danger of neurosurgery using Joimax technology.Yes, we are the only ones in the country so far, but there is confidence that with time such surgery will become the standard for all domestic medicine - progress advances itself.
We hope that this material was useful and gave some insight into how modern medicine has ways to help. Now you know that back pain is not normal, not forever and not necessary, even if you are 80. Enough to endure it.
- Spinal surgery is risky, threatened with disability and paralysis.
- Surgeons are ready to shred everyone, not even offering alternatives to the patient.
- A good masseuse will cure any back problem.
The warmer, the more often patients with complaints of back pain come to us at Medicine 24/7 . Someone has already opened the summer season, and someone was in a hurry to pump up by the summer.
And every day we get such results of examinations of these people, that they absolutely clearly show spinal surgery. She quickly and permanently relieve them of pain, "lumbago", "jamming" in the lower back, numbness of the limbs and more severe problems.
')
But Russian patients and, even worse, doctors - are trying to the last to avoid spinal surgery. It is still widely regarded as dangerous. And for safe neurosurgery, it is customary to go except to Germany and pay around 30,000 euros. Patients who are not ready for such expenses are forced to relieve the symptoms of hernia and stenosis with drugs and physiotherapy. But these measures do not remove the problem, but only make it possible to live with it, experiencing constant inconvenience, limiting oneself in movements, choice of hobbies, work and even posture for sleeping.
Now “Medicine 24/7” is the first and so far the only clinic in the country that performs endoscopic treatment of stenoses and hernias using the Joimax minimally invasive spinal surgery technology. On the German equipment with the price per operation is 7 times lower than in Germany.
Every day we prescribe people who, after a spinal surgery, leave us the next day on their feet, return to life without anti-inflammatory ointments and painkillers.
But most of the patients still continue to be afraid of surgery. Fears, most often, are based on those very myths about the inevitable danger of operations and the "conspiracy of surgeons." But doctors have long known the origin of the horror stories - as always, this is a lack of reliable information.
So today we will tell you how modern spinal surgery is done, whether the risks are really great, and how to live so as not to get to the table with the surgeon.
Why back hurts and why you can not tolerate
Almost every person over 20 at least once had a back pain. What is the reason?
The musculoskeletal system of Homo sapiens is well suited for erect walking, and in some places it even stores nostalgic memories of aging (for example, the broadest back muscles, which are now needed only for climbers and bodybuilders).

The broadest muscles of the back. Before any bodybuilder gorilla far.
Our main support - the spine - is made so as to spring up and soften the "recoil" when walking, running and other fast sudden movements. This is due both to its ventral (forward) and dorsal (backward) bends, and due to elastic “spacers” between the vertebrae - the intervertebral discs.

The spinal column is springy as a kind of hybrid of spring and shock absorber.
But a comfortable civilized life began, by historical standards, just yesterday, and life did not prepare us for this. It is not stipulated by human biomechanics that the body will sit motionless in a car for 3 hours a day and at a computer for 8-10 hours. But it is worth while rejecting the spine from the vertical or changing its natural deflection (for example, slouching) - the pressure on the intervertebral discs grows many times.

The pressure on the intervertebral discs in different conditions, the standing position is taken as 100% and is 5 bar (compare: in the car tire - 2 bar)
Nature did not expect that it would become fashionable to carry weights three times a week in the gym for the sake of beauty.

The load on the lumbar spine when exercising with a weight - up to 730 kg
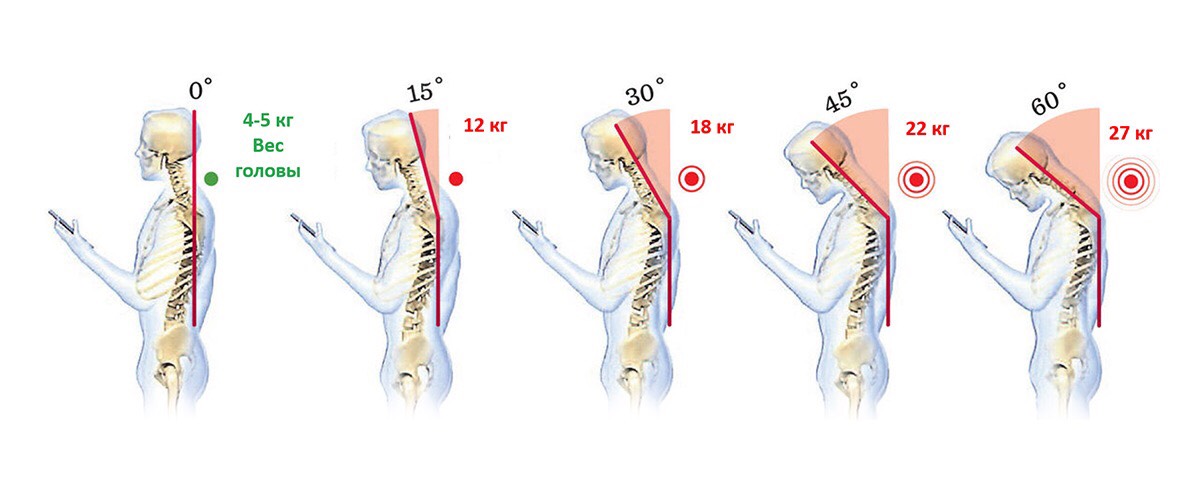
How many kilograms hang on your neck when you take out a smartphone?
The general conclusion is that the spine suffers for various reasons in almost all modern city dwellers. You or your acquaintances almost certainly have backache or neck pain, discomfort and numbness in the limbs, sharp headaches, tinnitus, and front sight.
But people are so accustomed to these symptoms in everyday life, that they simply adapt to them: they put pillows on them, turn over on the other side, or smear their backs with ointment from TV commercials.
Almost 90% of our patients, before coming with complaints to the clinic, engaged in self-treatment. Many have only exacerbated this problem. While a person lives with pain, changes, often irreversible, occur in his bone, cartilage, nervous tissue.
Pain - the first signal of such changes. Therefore, it can not be tolerated by anyone - it does not matter that you are still young and used to it, that you usually have “nothing serious”.
Going to a doctor in time and doing an MRI - this small effort can save you years of free movement and prevent really serious problems, even paralysis.
Hernia, protrusion, stenosis and other troubles
The most common cause of acute back pain, movement disorders and work of the limbs in patients of relatively young age (up to 50 years) is a herniated disc.
Here are healthy vertebrae and a disc in between.
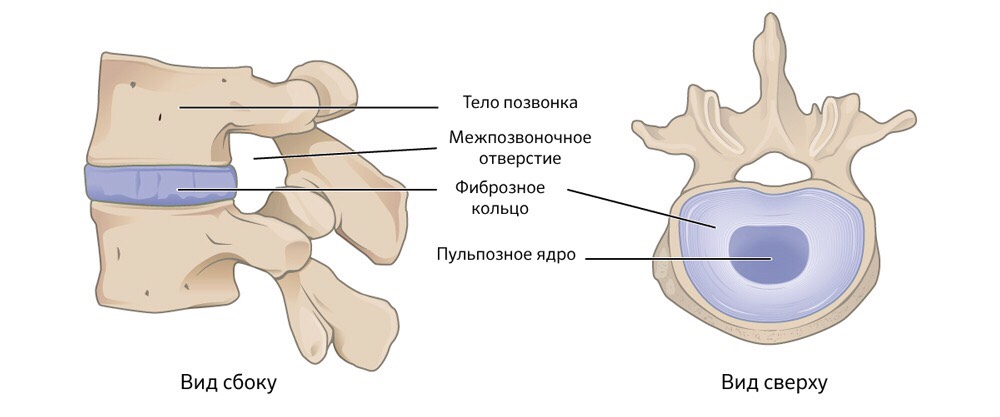
The structure and position of a healthy intervertebral disc
The disk consists of a dense fibrous fibrous ring, inside of which there is a gel-like structure - a pulp core. Top and bottom of the disc is covered with cartilage tissue.
Intervertebral discs do the work of shock absorbers when we move, sit for a long time, or stand. They prevent contact and abrasion of the vertebrae. If the intervertebral disc is subjected to strong pressure for too long and regularly, degenerative-dystrophic changes occur in it.
The fibrous ring is gradually deformed, becomes uneven thickness. And the pulpous core is still under stress. Where the thickness of the “crumpled” fibrous ring is minimal, the core pushes it outward, beyond the boundaries of the vertebral body. This protrusion in violation of the homogeneity of the fibrous ring is called protrusion.
It may not cause serious problems. If you take precautions, with protrusion, you can safely live a lifetime. But it is dangerous that the problems are already there, and without symptoms the person does not know about them and does not consider it necessary to protect the spine.
Then the protrusion increases with time. And where the fibrous ring is thin, it breaks there. The pulpous core is squeezed out. This is a hernia.
If it goes in the direction of the spinal canal, it squeezes the spinal cord or nerve roots passing there, causing great pain and disrupting nerve conduction.
Acute pain syndrome, immobilization (“wedged back”), disruption of the limbs, dizziness, and sometimes even temporary paralysis and dysfunction of some organs appear.

The development of the degenerative process in the intervertebral disc
Hernia can happen in both 20 and 70 years, but in old age (after 50 years) the cause of back and limb problems is often not a sharp, as in the case of hernia, but a gradual chronic process. Stenosis - narrowing of the spinal canal.
The reasons are common: age-related changes of intervertebral discs, their "wear". Consequently, destabilization of the vertebrae, reduction of the distance between them, overstrain of the facet joints. Plus a decrease in bone density and weakening of the muscles, making the vertebrae even worse withstand the load.
The body is trying to compensate for the instability of the spinal column, building up tight dense structures in "weak spots". Hypertrophy (enlargement) and ossification (ossification) of the yellow ligament, growth of the facet joints, formation of osteophytes (bone tissue growths) often develop. All these "additional fortifications" take place, narrowing the spinal canal.

The most likely causes of spinal stenosis
All this leads to pain syndromes, to neurogenic limp, etc.
How it is treated without surgery
If there is stenosis, protrusion or hernia, but there is no compression of the roots, impaired reflexes, movements and sensitivity, and there is only pain in the lumbar region, conservative treatment is prescribed. It includes three blocks - physiotherapy, physiotherapy exercises (LFK), and drug therapy.
Physiotherapy is a common name for a variety of therapeutic measures. These are methods of hardware exposure: tissue electrostimulation, magnetic therapy, electro- and phonophoresis; traction on a special rehabilitation simulator "Exarta"; soft manual techniques, massage.
Classes are added with an instructor LFK. He helps the patient to remove the musculo-tonic syndrome (prolonged spasms that damage the muscle fibers), teaches correct movements and exercises, monitors the correct technique of performance and the adequacy of the load, explains what cannot be done with this diagnosis.
Drug therapy is the third block. These are anti-inflammatory and painkillers that relieve muscular-tonic syndrome; vitamin therapy (milgamma, a complex of vitamins of group B); drugs that restore the conductivity of nerve fibers. These include tablets, injections, and topical ointments. Drug treatment has the main objectives: relieve spasm, remove pain, reduce swelling and improve blood circulation.
The main problem - conservative treatment removes the symptoms, but does not affect their source, the pathology itself. The main "mechanical" cause of problems does not go anywhere, a hernia or stenosis cannot "resolve" by themselves.
Physiotherapy can last for years. The patient becomes easier at the time. Then the aggravation returns, again you need to undergo a course of therapy. Conservative treatment requires an average of 1-2 times a year to invest in the back from 30,000 to 120,000 rubles. for medications and physiotherapy, so that you do not have to endure the pain and not get worse.
But conservative treatment is historically considered to be less risky than surgery aimed at eliminating the main problem. About 70% of cases of protrusions, hernias and stenoses are limited in testimony to conservative treatment today. So horror films about evil surgeons who never agree to send a patient to a pharmacy and to a massage, but only dragged into the operating room - this is nothing more than a folk exaggeration.
Spinal surgery: danger or necessity?
However, a problem arises when there are indications for surgery, but patients spend resources on ineffective treatment, and don’t go for surgery - because neither they nor, unfortunately, their doctor simply knows that operations can be safe. .
In the recent past, the only way to get to the spine was an open surgery. Such interventions are indeed associated with serious complications.
How to conduct open surgery
An incision is made at the level of the hernia, not less than 3-4 cm (up to 8) in length, the skin is dissected, the muscles are separated, access to the spine is released. Then a yellow ligament opens up: for this purpose, the pliers remove the bows of the underlying and overlying vertebra so that you can see the structures in the spinal canal. With a special hook, the nerve root is set aside, a hernia is cut.

The schematic image of the removal of the hernia with open surgery
If the operation is performed for stenosis, everything goes in a similar way, but a part of the ligaments and bone tissue of the vertebra is removed, sufficient to achieve decompression of the strangulated nerve roots - in other words, to give them additional space.

Open surgery for spinal stenosis
The main difficulty of the majority of open surgeries with resection of bone structures - after removal of parts of the vertebrae, destabilization of the spinal column occurs: the overlying vertebrae have nothing more to rely on. To correct the situation, pedicle clamps are inserted - from 4 to 6 screws are screwed in to keep the spine in the right condition. Implantation of any "iron" looks cool only in comics, but in life it is a risky event.

Titanium screws to ensure the stability of the damaged spine
Full recovery after an open operation takes 4-6 months, the patient cannot sit for a long time and moves with difficulty, needs rehabilitation with the help of physiotherapy, massage, and medications.
Consider possible complications during open surgery.
Irreversible damage to the nerve roots. To open the yellow ligament or resect part of the overlying / underlying vertebra, you need to forcefully press on the nippers. And even an experienced surgeon will not give a 100% guarantee that at this moment an instrument or bone fragment will not damage the nerve.
Durotomy. Damage to the dura mater around the spinal cord. Not a rare event during manipulations on the spine, which can lead to damage to the nervous tissue and the outflow of cerebrospinal fluid - liquorrhea. And this is again the compression of the roots and spinal cord, pain and movement disorders, the risk of developing meningitis.
The formation of scars and adhesions. Contact of nerve roots with air provokes excessive scar formation. And even if the operation was successful, the replacement of the nervous tissue in the root with the connective tissue of the scar eliminates the results of the operation and leads to a re-deterioration of the patient's condition.
Despite the complexity and risks of open operations, they are still regularly done around the world. The main reason for such a commitment to tradition is open operations that are undemanding to the technological equipment of the hospital. They do not need to buy expensive equipment and upgrade the skills of surgeons and medical staff.
Endoscopic operations require the purchase of new technology, training of doctors - and this is a serious expense.
An experienced neurosurgeon will understand the technology of endoscopic interventions for a week, but for this he needs to go to training with German or American colleagues, and then himself conduct at least 30 operations on Joimax or similar equipment. In Russia, such a technique is almost impossible to find: it costs 20,000,000 rubles - an adequate price for complex high-tech technologists, but unrealistically huge amounts of money for domestic hospitals.
Therefore, patients with hernia, stenosis, and radicular symptoms: pain, impaired reflexes, and movements — who have not received adequate help for years, come to Medicine 24/7 regularly. Although our neurosurgeons could have relieved them of the problem for a long time, it was less traumatic, quickly and definitively.
How to operate the spine without incisions?
Many modern operations become closed, endoscopic: special thin tubes-manipulators with micro tools and video cameras at the ends are inserted through the punctures in the skin - the doctor sees everything he does without risking damage to bone structures, nerve tissues or muscles. For neurosurgery with its high risks, this is especially useful, and here minimally invasive endoscopic access becomes the quality standard.
True, this requires sophisticated modern equipment. It is produced by only a few companies, mostly German, and even they are not equally good. Neurosurgeons of our clinic, while they were going to study in Germany, tried all the available technology options, and stopped at Joimax - this equipment allows you to work on all spinal sections and solve all problems.
The main advantage of endoscopic operations is minimal trauma. Access to the affected area occurs through natural anatomical windows between the bone structures of the spinal column: intralaminar (between the vertebral arches) or transforaminally (through the intervertebral foramen). In this case, the doctor does not violate the biomechanics of the spine, does not open the spinal canal, does not remove part of the vertebra to get to the place of nerve compression.

Neurosurgeon does not look at the patient during endoscopic surgery.

He looks at the monitor, where he sees everything that happens from the inside.
An MRI / CT scan is performed before the operation. Sometimes functional images are assigned to see if there is no fidez (displacement of the vertebral bodies relative to each other) but, as a rule, MRI and CT are sufficiently informative. By the time of surgery, the doctor understands exactly what will happen and how.
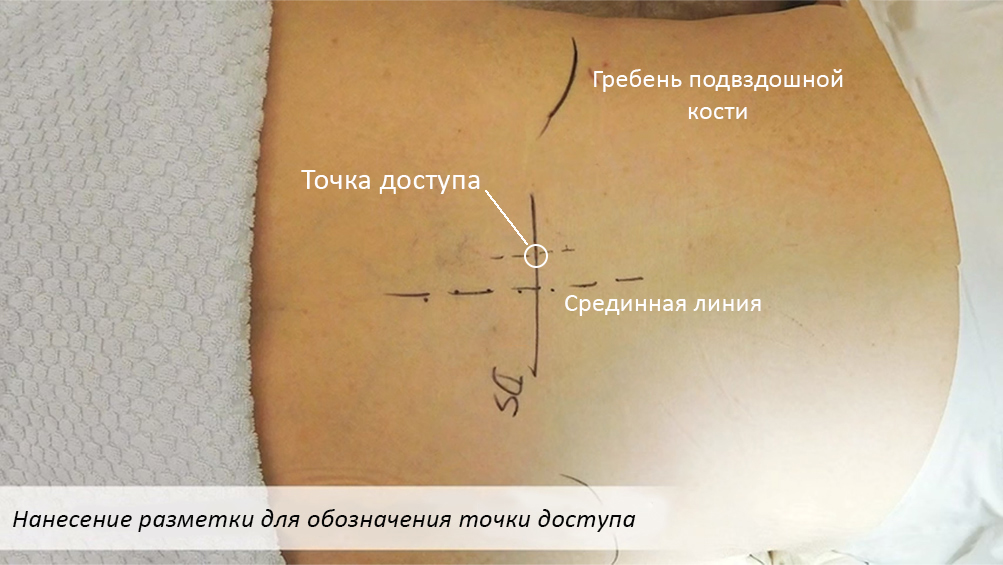
Reconnaissance on the ground - the access point is clear to the millimeter
A micro-cut is made at the exact location. Special tubes are introduced into it, gradually gently widening the hole and serving as guides for endoscopic instruments. The accuracy of administration at this stage is constantly monitored by X-rays. The working tube remains in the patient until the end of the operation.
And then an endoscope is inserted into the tube: a special instrument, which, in fact, is also a hollow tube. At the end of the endoscope is a video camera and a light source, and a channel for all other instruments passes through it.The endoscope is also inserted once at the beginning of the operation, and other instruments are delivered to the scene of action through it as needed.

Endoscope and instrument inserted through it.
A cable is connected to the endoscope through which the image from the endoscope camera is transmitted to the monitors in the operating room. The neurosurgeon sees all the capillaries, vessels, nerves, ligaments, bones with an increase of more than 50 times (compare: an ordinary operating microscope increases 20-30 times).
Through the endoscope, one can literally with jeweler precision remove excess tissue that causes a narrowing of the lumen of the spinal canal and compression of the nervous structure. To perform a resection of soft and hard tissues, grind off “extra” bone structures with a diamond cutter, rinse the operated area — moreover, the cut-off parts of the tissues, bone dust and fluid are removed through the same endoscope.

The process of resection of a hernia with special forceps inserted through an endoscope. In the upper right corner shows how this moment looks on the x-ray.
The whole operation takes an average of an hour. The longest case in the practice of our clinic is 4 hours, removal of complex stenosis in the lumbar region. A large number of growths took time to carefully remove them: the grinding of bone tissue with a diamond cutter is a delicate and gradual process.
But the main thing, of course, is not that it is more convenient, faster and easier for a neurosurgeon to work using Joimax technologies. The benefits are in patients. Treatment of stenosis or hernia with minimally invasive endoscopic surgery is devoid of complications, risks, and simply the inconvenience inherent in open surgery.
Blood loss is minimal. With an open operation, the muscles are opened, the bone is bitten off, the bleeding will necessarily be (yes, the bones also bleed). When working with a high-speed cutter, there is no blood. The cutter turns the bone into dust, and the damage to the vessels is simply "sealed."
Visual inspection reduces the risk of accidental damage.If, for example, inadvertent damage to the membrane occurs around the spinal cord, the doctor will see it immediately and eliminate it, avoiding complications such as liquorrhea (the expiration of the CSF).
The absence of contact with air eliminates the pathological scarring of the nervous tissue and the formation of adhesions.
Accessibility for patients with diabetes, obesity, diseases of the cardiovascular system. Open operations are contraindicated in them, since will cause serious complications. With endoscopic complications will not. In Medicine 24/7, such patients receive help when conservative treatment has completely stopped working. In other clinics, these people, most likely, have already been refused. But Joimax technology is safe even for them, and, most importantly, effective. People stop to suffer.
Rapid rehabilitation. During endoscopic spinal surgery there are no massive operative injuries, after the operation there are no drains left, metal implants - only a 1.5 cm suture. The patient gets up after 12 hours, and within a few days returns to the usual life.
Maybe to massage, and not to operate?
It is logical that people are still afraid of surgery, even minimally invasive, but sometimes they choose on their own much more dangerous methods of treatment, mistakenly considering them a soft alternative.
Private “Healthy Back Centers”, manual and osteopaths today are fashionable and in demand, but may be more risky than an operation.
Often they save time on diagnosis. Everyone is offered the same thing, regardless of diagnoses, the level and nature of pain syndromes. Bad manual therapists treat patients without an MRI or at least x-rays.
Remember, a “hands-on” treatment can aggravate the problem. Patients regularly come with exacerbations and deterioration of the situation after a visit to a “private man” therapist or to a dubious “spinal health clinic”. When, for example, a person with a hernia of the cervical region (an absolute contraindication for massage) begins to "crack the vertebrae," and he comes to us by ambulance.
Manual therapy is great, but careful, only as directed by a doctor, only after an accurate diagnosis. If the "doctor" puts you on a massage table, not interested in the history, it is better to find another.
Summary
Even 50 years ago, people were afraid of dentists, and they could be understood, but now the treatment of a tooth does not cause pain and takes minimal time at any clinic. With spinal surgery the same situation.
For Medicine 24/7, safe, accurate and efficient endoscopic neurosurgery has been a familiar standard for several years, but patients and even many of our industry colleagues simply do not know that safe radical treatment is available in Russia. And they continue to consider the danger of spinal surgery in general, although the risks of endoscopic intervention cannot be compared with the risks of open operations.
Often the danger of neurosurgery using Joimax technology.Yes, we are the only ones in the country so far, but there is confidence that with time such surgery will become the standard for all domestic medicine - progress advances itself.
We hope that this material was useful and gave some insight into how modern medicine has ways to help. Now you know that back pain is not normal, not forever and not necessary, even if you are 80. Enough to endure it.
Source: https://habr.com/ru/post/452916/
All Articles