Cute 3D bones: hyperelastic bone material for plastics of skull defects

We have about 205 of them, in total they weigh about 5-6 kg and every 10 years they are completely updated at the cellular level. And then there is an idiomatic expression that says everyone has it in the closet. This, of course, is about the skeleton and the bones that make it up. Injuries related to bone damage are among the most common in the world. Sometimes such injuries do not require bone treatment, but replacement. Bone transplantation is associated with a number of dangers for the patient, including subsequent pain, infection, bleeding, damage to the conjugated tissue, etc.
Some scientists believe that the key to successful bone graft lies in the use of printed bones, which will be ideally suited to a specific patient and will be free from defects. How did the scientists print the bones, what was used for this and what results did the implant operation show on the rat? We learn about it from the report of the research group. Go.
')
The basis of the study
Methods for treating bone injuries have not changed much since ancient times. Scientists have even analyzed 36 skeletons of Neanderthals, which were signs of fractures. Of these, only 11 can treat these injuries as unsuccessful.
However, such success of treatment at all times does not apply to all types of fractures. Some injuries were successfully and successfully treated without sufficiently modern medical equipment, knowledge and techniques.
Currently, allografts or alloplastic materials are often used in bone transplantation.
Allotransplantation * - organ transplantation from person to person (from an individual of one species of an individual of the same species).These methods are quite advanced, but not all-powerful. Cranio-maxillofacial defects (congenital, oncological or traumatic origin) are quite complex. In such cases, implants are needed that are specific to a particular patient. Therefore, they cannot be taken from the donor, but must be manufactured. In such cases, cranioplasty is used, however, the implant will not have regeneration and will not grow with the patient's other bones. Bone spongy substance, demineralized bone matrix, synthetic bone chips or bone putties are used to fill in the defect area. But these materials are not porous and have limited bound porosity. Because of this, cell surface migration and vascularization (vascular formation) of cells is reduced, which can lead to encapsulation * , and not to tissue integration. As a result, the risk of infection is greatly increased.
Encapsulation * - the formation of a capsule around a foreign body in the body.Researchers suggest using three-dimensional printing, because this method allows you to make an inexpensive implant that will ideally fit a specific defect in a particular patient.
Researchers also note that biomedical three-dimensional printing still lacks high-performance materials that will combine the simplicity of manufacturing, use in printing and biological functionality. This means that you need to create your own material, of course.
Hyperelastic Bone
And the name of this new material is “hyperelastic bone” (hyperelastic bone material). This osteoregenerative material is manufactured by extrusion of hydroxyapatite (solid, 90% of the total mass) and poly (lactic glycolic acid) (liquid substance, 10% of the total mass) at room temperature (liquid substance, 10% of the total mass) without the need for sintering * , curing * or other forms of physico-chemical stabilization.
Sintering * - the process of making solid and porous materials from fine powdered base at elevated temperatures and / or high pressure.
Curing * is an irreversible process of converting liquid reactive oligomers and (or) monomers into solid non-meltable and insoluble crosslinked polymers.The resulting three-dimensional printed frame has good elasticity and high absorption. In addition, the framework causes osteogenic differentiation * of human mesenchymal stem cells obtained from bone marrow without the addition of osteoinducing catalysts.
Cell differentiation * is the process of forming a specialized cell phenotype that reflects its functions. Exaggerated, the employment of the cell, which previously did not have the exact profession.At the same time, the hyperelastic bone did not cause a negative immune response, became vascularized and integrated with the surrounding tissues, supporting the growth of the new bone. Another achievement is the ability to transfer transduced human adipose stem cells through a printed implant.
Next we will take a closer look at the results of practical tests. Scientists conducted a comparative analysis of the osteoregenerative ability of the hyperelastic bone and the commercial variant (autologous bone) with critical-sized cranial defects in rats. But first, a little about the preparation for the experiment and how the test material and implant were made.
Hyperelastic Bone Making
As we already know, the skeleton of the hyperelastic bone was made of hydroxyapatite and poly (lactic glycolic acid).

BioPlotter Printer
All samples were printed using the EnvisionTEC BioPlotter Manufacturing printer. The thickness of the sheets (5x5 cm), consisting of 5 layers of 120 μm, was totally 0.6 mm. Further, round (8 mm in diameter) blanks were extruded from the sheets using a biopsy stylet. The resulting blanks were washed and sterilized.

Image number 1: the process of making implants.
Implant surgery
Laboratory Spreg-Dawley rats, males weighing approximately 500 grams each, acted as experimental subjects.
During the operation, the subjects were under general anesthesia (2% isoflurane / 100% oxygen). A sagittal incision (1.5 cm) was made between the lambdoid and coronal sutures to expose the skull. An artificial cranial defect of 8 mm in diameter was created using a hand drill with a trepan (a needle with a cutter or a drill to form holes in dense tissues).
The experimental were divided into 4 groups:
- 7 individuals - negative control group (without implant on the defect);
- 6 individuals - positive control group (with an autologous bone as an implant);
- 6 individuals - study group No. 1 (with a frame of poly (lactic glycolic acid) as an implant);
- 10 individuals - the investigated group No. 2 (with hyperelastic bone as an implant).
This spoiler contains a photo of the experimental during the operation (please do not look at the nervous nerves, the process was described in text form earlier).

After implantation (or without it), the periosteum and skin were closed using a movable absorbable suture, and the anesthetic was administered to the test subjects. The experimental were contained in cells of two. Access to water and food was unlimited.
Samples of skulls were analyzed by means of a cone-beam computed tomography. Areas of interest were cut from the bones of the skull, placed in 70% ethanol and scanned with a microcomputer tomograph. Then, using medical image analysis software (Mimics Medical 19.0), scientists investigated in more detail the areas of the skull where implants were inserted.
After micro-computed tomography, the samples were cut in half for histological analysis and visualized by scanning electron microscopy. The degree of regeneration was also evaluated after 8 and 12 weeks.
And now we proceed directly to the results of observations.
Research results
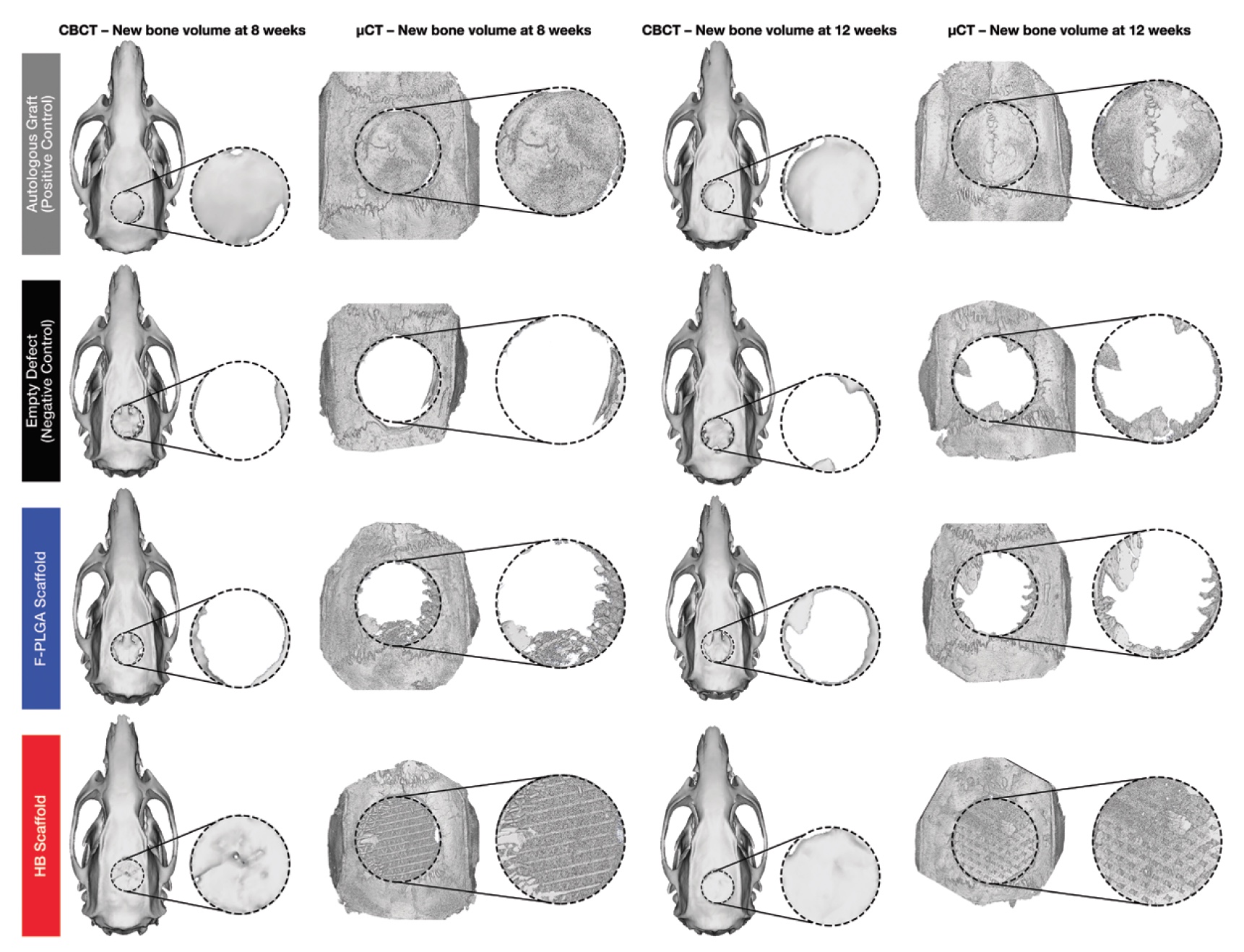
Image number 3a: gray - with autologous bone; black - without implant; blue - with an implant of poly (lactic glycolic acid); red - with hyperelastic bone.
The image above ( 3a ) shows three-dimensional reconstructions of cone-beam and micro-computed tomography. The amount of regenerated bone tissue was determined by the amount of mineralized bone as a fraction of the total volume of tissue of interest. Bone volume per total volume for hyperelastic bones, poly (lactic glycolic acid) and for the negative control group were normalized relative to the bone volume for the total volume for the positive control group (with autologous bone). Thus, a comparative analysis of the performance indicators of all variants of the implant was carried out.
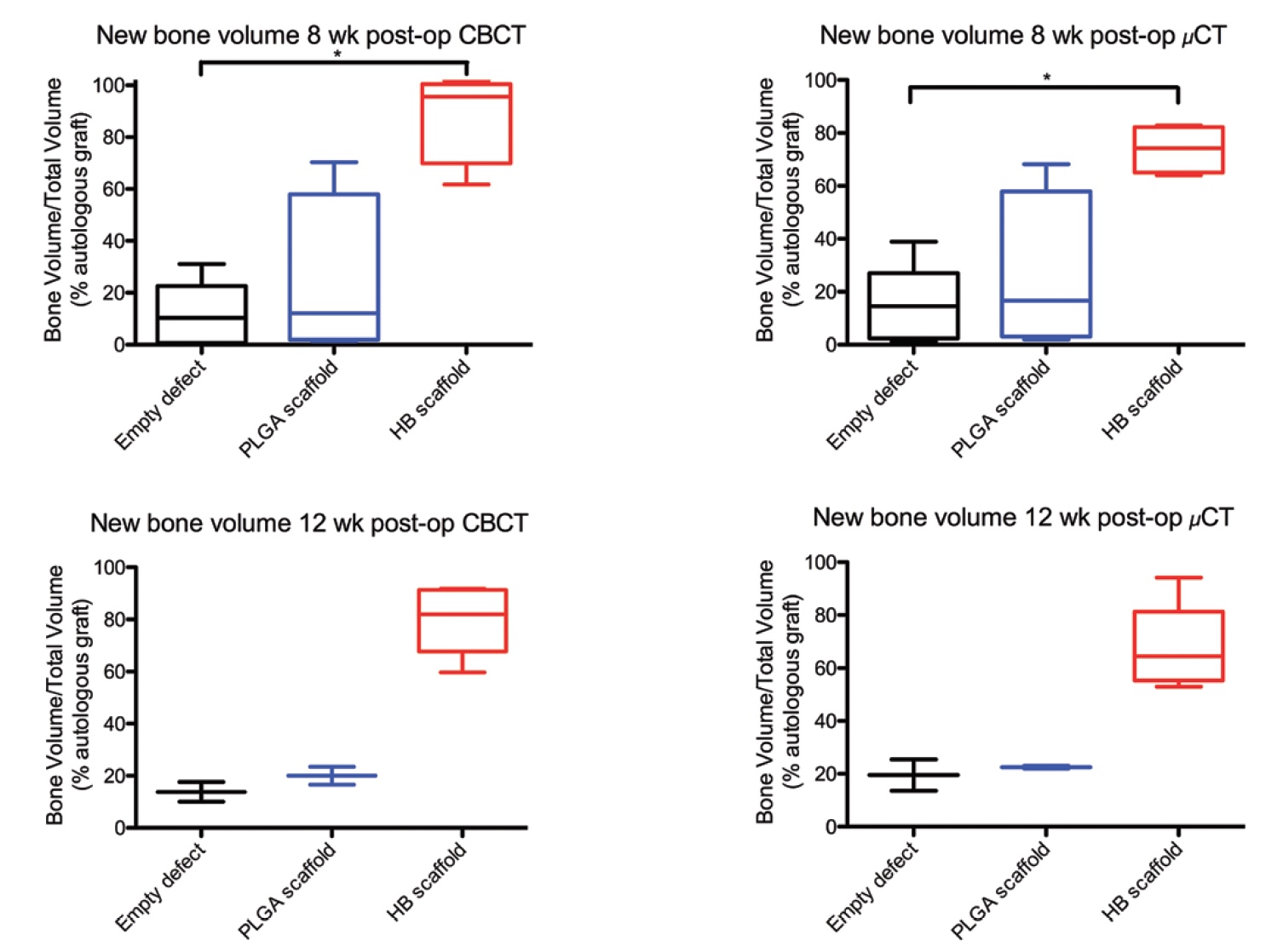
Image number 3b
Cone-beam and micro-computed tomography showed an increase in the number of mineralized bone matrix in defects treated with hyperelastic bone implants ( 3b ).
According to the data of a cone-beam tomography, the volume of mineralized bone in the case of the use of hyperelastic bone implant was 55.7% at week 8 and 57.0% at week 12 of observations. According to the data of micro-computed tomography - 36.1% at week 8 and 37.1% at week 12 of observations. This is the data before normalization.
This was followed by normalization to the volume of mineralized bone in the case of autologous grafts. Now it became clear that the volume of regeneration with the use of hyperelastic bone was 95.6% and 82.0% (8th and 12th week of observations) of the volume of the positive control group (with autologous bone). And microcomputed tomography gave the following results: 74.2% and 64.5% (8th and 12th week of observations).
The use of exclusively poly (lactic glycolic acid) as a material for implantation turned out to be rather ineffective: 16.6% and 22.5% (8th and 12th week of observations) of the volume of the positive control group. The ineffectiveness of this method is also confirmed by the fact that its results do not differ much from the results of the negative control group, which had no implants at all: 10.3% and 13.8% on cone-beam tomography and 14.5% and 19.5% on micro-computed tomography.
Comparison of the results of the test material (hyperelastic bone) with the results of the negative control group showed a difference in the volume of mineralized bone by 7.81 times at week 8 and 5.75 times at week 12 in favor of hyperelastic bone.
Thus, from the point of view of the volume of regeneration, the use of hyperelastic bone is almost comparable with the use of commercial variants of implants with autologous bone.
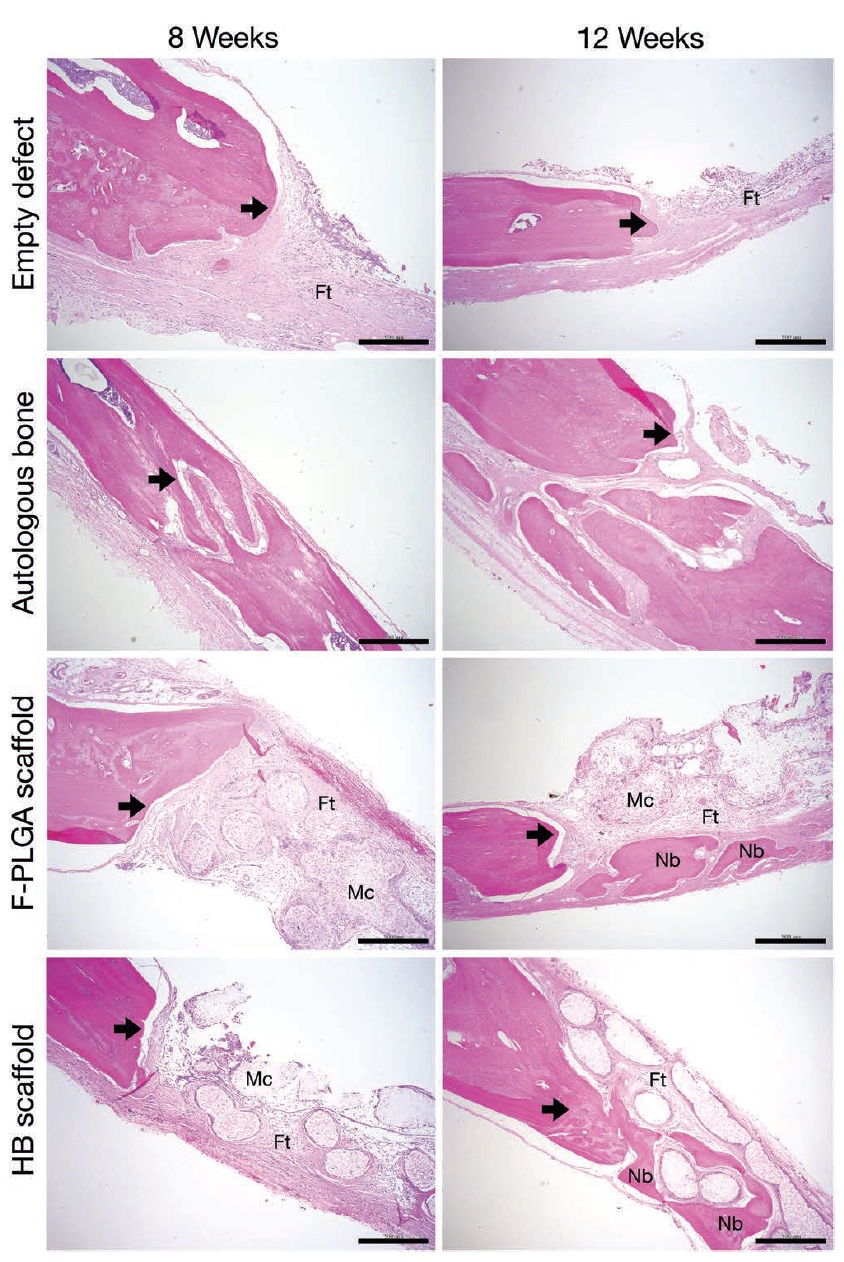
Image number 4: arrows - defective edge; Ft - fibrous (fibrous) tissue; Mc - membrane-cell component; Nb is a new bone.
Conducted histological analysis only confirmed the data of cone-beam and micro-computed tomography. Scientists have identified the edges of defects, and the formation of new bone was specially painted using eosin for better visualization.
In the case of a negative control group, fibrous tissue was observed, but the formation of a new bone was minimal (top row in image No. 4). Samples with poly (lactic glycolic acid) also could not boast a large volume of newly formed bone (third row).
But the samples where the hyperelastic bone was applied, on the contrary, showed the formation of mineralized bone tissue on the surface of the edges of the defects (4th row). At week 8 of observations in the places of defects, fibrous tissue and membrane-cell components inside the implant appear, and on the 12th week, the formation of a new bone begins around the implant framework elements.

Image number 5
And finally, the analysis of SEM (scanning electron microscope) images of samples with hyperelastic bone at 12 weeks of observation showed the formation of close cellular tissue contact with the material inside the implant.
For a more detailed acquaintance with the nuances of the study I recommend to look into the report of scientists .
Epilogue
In this work, scientists have demonstrated a new type of osteogenic biomaterials that allow you to create implants for the treatment of bone defects. Scientists call the most important features of their offspring: ease of implantation, ease of manufacture, high efficiency, low production cost and customization of the implant for a specific patient.
Hyperelastic bone is really very elastic and can take the necessary form both in the manufacturing process and at the time of implantation, which greatly facilitates this process. Ceramic and polymer ceramic implants can not boast.
But even this is not the most important advantage. A high degree of bone regeneration and implant survival is much more important. Already 4 weeks after implantation, an active process of bone tissue mineralization begins.
Scientists also note that such speed and efficiency are extremely important in case of sufficiently large defects (as was demonstrated during practical experiments).
The use of such technology can greatly simplify the life of both doctors and patients. Individuality of treatment, speed of production, implantation and quick recovery without side effects - this is an excellent advertisement for a new technology. In the future, scientists intend to conduct a few more experiments, to study the process of regeneration in more detail and to improve their invention.
However, it is worth noting that the presence of such innovations does not mean that you can break bones to the left and to the right. So the security rules have not been canceled.
Unforgiving off-top:
Yes, today is not Friday and not time for off-stamp, but I could not resist. :)
Corpse Bride (2005, directed by Tim Burton)
Thank you for your attention, remain curious and have a good working week, guys. :)
Yes, today is not Friday and not time for off-stamp, but I could not resist. :)
Corpse Bride (2005, directed by Tim Burton)
Thank you for your attention, remain curious and have a good working week, guys. :)
Thank you for staying with us. Do you like our articles? Want to see more interesting materials? Support us by placing an order or recommending to friends, 30% discount for Habr's users on a unique analogue of the entry-level servers that we invented for you: The whole truth about VPS (KVM) E5-2650 v4 (6 Cores) 10GB DDR4 240GB SSD 1Gbps from $ 20 or how to share the server? (Options are available with RAID1 and RAID10, up to 24 cores and up to 40GB DDR4).
VPS (KVM) E5-2650 v4 (6 Cores) 10GB DDR4 240GB SSD 1Gbps before summer for free if you pay for a period of six months, you can order here .
Dell R730xd 2 times cheaper? Only we have 2 x Intel TetraDeca-Core Xeon 2x E5-2697v3 2.6GHz 14C 64GB DDR4 4x960GB SSD 1Gbps 100 TV from $ 199 in the Netherlands! Dell R420 - 2x E5-2430 2.2Ghz 6C 128GB DDR3 2x960GB SSD 1Gbps 100TB - from $ 99! Read about How to build an infrastructure building. class c using servers Dell R730xd E5-2650 v4 worth 9000 euros for a penny?
Source: https://habr.com/ru/post/452726/
All Articles