SENS-diagnostics. Biomarkers of mitochondrial dysfunction and oxidative stress
With this review, we are starting a series of articles describing potential biomarkers for the SENS diagnostic panel of aging.
The concept of SENS (Strategies for Engineered Negligible Senescence, a strategy for achieving negligible aging by engineering methods) was proposed by the British gerontologist Aubrey de Gray. The idea of the concept is the need to develop and apply technologies to combat aging and age-related diseases in order to "repair" the accumulating damage in the body. The goal of our review of potential biomarkers is to create a SENS diagnostic panel for aging.
Why do I need SENS diagnostics?
')
SENS concept includes 7 sections. The first item to consider is the mitochondrial dysfunction (or MitoSENS).
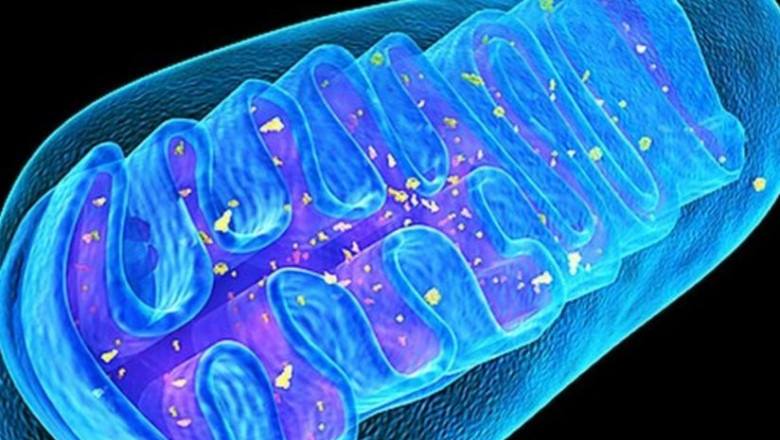
Mitochondria are tiny organelles of eukaryotic organisms (with the exception of Giardia inhabiting the intestines of chinchillas), which produce energy for all biochemical processes. According to the most popular version, the mitochondria had long been independent units of life, purple photosynthetic bacteria, but in the process of evolution were absorbed by ancient microorganisms, archaea, and began to produce energy for them. Each cell can contain more than a thousand mitochondria, for example, the heart muscle cells have up to 5,000 mitochondria. Molecular motors, ATP synthase, embedded in the inner membrane of mitochondria, rotate under the influence of a stream of protons and synthesize the main source of energy - adenosine triphosphoric acid, ATP. It is estimated that the body of an adult synthesizes and consumes about 40 kg of ATP per day.
Mitochondria, unlike other organelles, have their own 2-10 copies of DNA, mtDNA. In the process of energy production, mitochondria generate toxic "waste" - reactive oxygen species (ROS), which can damage both other molecules and various cellular structures and, above all, mitochondria themselves, which can cause mutations in mitochondrial DNA and adversely affect the overall energy balance of the body. Thus, mtDNA deletions (precipitations) of mtDNA are able to multiply rapidly and fill the cellular space, causing sarcopenia and neurodegeneration. “Damaged” mitochondria begin to produce even larger amounts of ROS, leading to an increase in oxidative stress, which, in turn, can cause the development of various pathologies, premature aging and cell death.
An interesting fact related to oxidative stress. It was found that there is a clear correlation between the level of fatty acid saturation in membranes and the life expectancy of animals: the longer the membrane of unsaturated acids, the shorter the lifespan of the animal. Spanish biologists have traced such a sequence showing an increase in the life span while simultaneously decreasing the content of docosahexaenoic ω-3 fatty acid in the membranes: mouse → rat → rabbit → man → whale [1].
This pattern is easy to explain, because unsaturated fatty acids are the main "victims" of lipid peroxidation. Thus, the lipid composition of animal cell membranes, which is characterized by a longer life expectancy, demonstrates the golden mean: a small amount of completely unsaturated docosahexaenoic 22: 6 ω-3 fatty acids and the predominance of less unsaturated linolenic 18:03 ω-3 fatty acids, which it creates the same balance, providing both protection against ROS exposure and preserving the necessary fluidity of the membrane.
In addition to the lipid composition of animal cell membranes, the proportion of more thermodynamically stable guanine and cytosine among all mtDNA nucleotide residues also correlates with the maximum mammalian species lifetime [2].
The creators of the SENS concept see the solution to the problem of mitochondrial dysfunction in the transfer of "backup copies" of mitochondrial genes into the nucleus, where they cannot be damaged by ROS generated in mitochondria. Thus, even if the original genes in mtDNA are damaged, the backup copies in the nuclear DNA will be able to supply the proteins necessary to maintain normal energy production. This approach is called allotopic protein expression. Human mtDNA contains only 37 genes, of which only 13 encode proteins necessary for mitochondria, the rest (over 1000) of proteins coordinating the work of mitochondria are encoded in nuclear DNA. According to the authors of SENS, the transfer of the main mitochondrial genes into the nucleus was carried out by evolution precisely for this purpose - to protect them from the damaging action of ROS.
The idea of SENS authors about the evolutionary transfer of mitochondrial DNA into nuclear to protect mtDNA from harmful factors and, thus, prolong life, is confirmed in studies devoted to the analysis of the NUMT (nuclear mitochondrial DNA segment). The term NUMT refers to mtDNA fragments transferred to nuclear DNA. A comparative analysis of 17 species of animals with fully sequenced mitochondrial and nuclear genomes showed a significant positive correlation between life expectancy and the number of NUMT sequences [3]. It now remains to find an engineering solution for transferring backups of the remaining 13 mtDNA genes.
But there are alternative approaches to improving mitochondrial function. And one of them is transplantation of mitochondria from the outside. Successful “sharing” of alien mitochondria in experiments with animals has been described. Thus, mitochondrial transport was used in animal models for acute lung damage, cardiovascular diseases, and Parkinson's disease. Mitching of mitochondria can be accomplished in several ways: first, direct administration of isolated mitochondria (local administration), when isolated mitochondria are introduced directly into the cells of the damaged area; secondly, systemic administration, when the mitochondria are injected into the general circulation, and then they are distributed throughout the body. The results indicate the prospects for mitochondrial transplantation in the treatment of a number of diseases [4].
At the same time, it would be logical to find potential biomarkers for determining oxidative stress caused by mitochondrial dysfunction.
Oxidative stress is an imbalance between oxidants (active forms of oxygen) and antioxidant protection in the body towards oxidants. In cells, oxidants actively interact with biomolecules (phospholipids, proteins and nucleic acids). As a result, these biomolecules are irreversibly damaged, which leads to cellular dysfunction and, as a result, various pathologies in the body and cell death. One of the most popular theories of aging, free radical, proposed by D. Harman in the 1950s, sees this as the main mechanism of aging.
Molecules formed during oxidation can serve as biomarkers. Their analysis is used to quantify oxidative stress in humans. High concentrations of oxidative stress biomarkers are determined not only in age-related or degenerative diseases, such as Alzheimer's disease, hypertension, type 2 diabetes, or several types of cancer, but also in chronic obstructive pulmonary disease, smoking and living in ecologically unfavorable areas.
One of the most important biomarkers of oxidative stress is 8-iso prostaglandin F2α (8-isoprostane). 8-isoprostane is formed by non-enzymatic oxidation of phospholipids of cellular biomembranes, namely arachidonic acid. This prostaglandin-like substance causes constriction of blood vessels and bronchi, reduces blood flow in the kidneys, affects platelet aggregation and, thus, participates in the pathology of several diseases. Normal values of 8-isoprostane in healthy people are 11 ± 4 pg / ml [5].
Also recognized as a biomarker of lipid oxidation is malonic dialdehyde (MDA), which is formed during lipid peroxidation by free radicals and the breakdown of poly-saturated fatty acid molecules. The increased concentration of MDA in the serum serves as a marker not only of oxidative stress, but also the degree of endogenous intoxication. Therefore, an increase in the concentration of MDA in plasma is observed in smokers, as well as in people who abuse alcohol. MDA forms Schiff bases with amino groups of the protein, resulting in insoluble lipid-protein complexes (wear pigments or lipofuscin). MDA is determined in samples of many biological fluids: serum, plasma, urine, condensate of exhaled air. The concentration of MDA in the serum of healthy people (normal) is less than 1 µmol / l [6].
With the oxidation of amino acids that make up proteins, a number of potential biomarkers of oxidative stress are formed: o-tyrosine, 3-chlorothyrosine, and 3-nitrotyrosine.
Physiologically in the body, endogenous tyrosine is formed by the enzymatic oxidation of phenylalanine with phenylalanine hydroxylase. o-tyrosine (o-Tyr) and m-tyrosine (m-Tyr) are formed during the oxidation of phenylalanine with active forms of oxygen. o-Tyr and m-Tyr are not naturally occurring amino acids and are considered biomarkers of oxidative stress. High concentrations of o-Tyr and m-Tyr were found in patients with cataracts, and elevated o-Tyr was found in the blood plasma and urine of patients with type 2 diabetes. 3-Chlorothyrosine (3-ClTyr) is formed in free radical processes during the reaction of hypochlorous acid (HClO, a derivative of hydrogen peroxide) and p-tyrosine.
The formation of 3-ClTyr plays an important role in the cardiovascular system, since it is associated with the development of atherosclerosis. 3-ClTyr promotes the migration of smooth muscle cells of the human aorta (the main mechanism for the formation of vascular lesions), and elevated levels of 3-ClTyr in inflammatory conditions may contribute to vascular diseases. 3-nitrotyrosine (3-Notyr) is formed under oxidative stress by nitration of tyrosine with aggressive phagocytic protein myeloperoxidase (MPO). Such nitration adversely affects the function of the protein. Higher concentrations of 3-Notyr were found in the cerebrospinal fluid of Alzheimer's patients (11.4 ± 5.4 nM in patients and 1.6 ± 0.4 nM in the group of healthy volunteers), as well as in people with arthritis, atherosclerosis and hypertension [5].
Also, under the action of ROS and HClO on proteins, various oxidation products of proteins (AOPP) are formed. Such proteins do not perform their functions and can cause significant harm. AOPPs are produced by the myeloperoxidase-hydrogen peroxide system. Higher concentrations of AOPP have been detected in the plasma or urine of patients with acute coronary syndrome or active ulcerative colitis. Plasma levels of 60–70 nM are considered normal indicators of AORP in healthy people [5].
Well-known biomarkers of nucleic acid oxidation are 8-hydroxyguanosine (8-OHG) and 8-hydroxy-2'-deoxyguanosine (8-OHdG). 8-OHdG is the main product of DNA oxidation. 8-OHG is formed by the oxidation of RNA. A higher concentration of 8-OHdG is found in patients with Alzheimer's disease, arthritis, atherosclerosis, cataracts, hypertension, osteoporosis, and type 2 diabetes. 8-OHdG is also considered a potential biomarker for smoking-related cancer (for example, lung cancer). 8-OHG can be detected in Alzheimer's patients, and it has been shown that oxidative damage to RNA is higher than DNA damage. Blood concentrations of 8-OHdG in healthy people are 1.09 ± 0.52 nM, and levels of 8-OHG (in the cerebrospinal fluid) are 97 ± 32 pM [5].
Another biomarker that determines mitochondrial dysfunction and oxidative stress is the number of copies of cellular mtDNA (there is also extracellular mtDNA, which enters the blood during cell breakdown and its level increases with age). So, it is known that the number of cellular mtDNA decreases with age, and in men it is more than in women. A lower mtDNA count is also significantly associated with the development of senile asthenia (frailty). The number of copies of mtDNA can also be an effective prognostic marker for all-cause mortality, cardiovascular, cancer and respiratory diseases [7].
Endogenous antioxidants, such as glutathione, cysteine, uric acid and ubiquinol, also have potential for use as biomarkers of mitochondrial dysfunction and oxidative stress. When interacting with active forms of oxygen, endogenous antioxidants are oxidized, but then restored again with the help of special enzymes. Therefore, in the body, antioxidant molecules are present in two forms: reduced form (antioxidant) or oxidized (after reaction with oxidants). Using the chromatographic method, it is possible to record the ratio of reduced and oxidized forms of antioxidants and thus determine the degree of oxidative stress [8].
Biomarkers of mitochondrial dysfunction and oxidative stress:
1. 8-isoprostane.
2. Malonic dialdehyde
3. O-tyrosine, 3-chlorothyrosine, 3-nitrotyrosine.
4. Protein Oxidation Products (AOPP).
5. 8-hydroxyguanosine (8-OHG)
6. 8-hydroxy-2'-deoxyguanosine (8-OHdG).
7. Cellular mtDNA (its number and the presence of mutated variants with deletions)
8. Endogenous antioxidants (glutathione, cysteine, uric acid, ubiquinol).
Review authors: Denis Odinokov, Alexey Rzheshevsky.
The concept of SENS (Strategies for Engineered Negligible Senescence, a strategy for achieving negligible aging by engineering methods) was proposed by the British gerontologist Aubrey de Gray. The idea of the concept is the need to develop and apply technologies to combat aging and age-related diseases in order to "repair" the accumulating damage in the body. The goal of our review of potential biomarkers is to create a SENS diagnostic panel for aging.
Why do I need SENS diagnostics?
')
- To enable a person to objectively evaluate what happens to his body in the process of aging from the point of view of SENS.
- See the individual risks of certain types of damage associated with aging.
- Assess the effectiveness of the developed methods of rejuvenation. See how physical activity, diet, day regimen, dietary supplements, drugs act in terms of a strategy to slow down aging.
- Compare with other diagnostic panels of aging, and complement their development.
- Provide data on changes in parameters for scientific research.
- Decide on the financing of scientific research based on the most interesting and sensitive risks.
- Find like-minded people to solve biological problems that have arisen as a result of understanding their own state of the organism from the point of view of SENS.
SENS concept includes 7 sections. The first item to consider is the mitochondrial dysfunction (or MitoSENS).
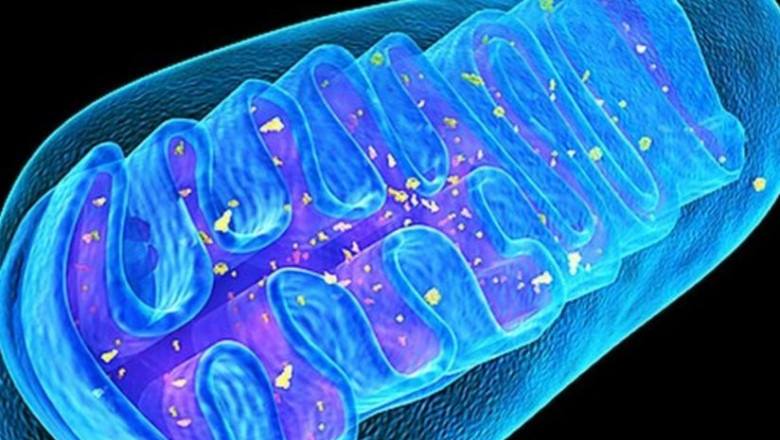
Mitochondria are tiny organelles of eukaryotic organisms (with the exception of Giardia inhabiting the intestines of chinchillas), which produce energy for all biochemical processes. According to the most popular version, the mitochondria had long been independent units of life, purple photosynthetic bacteria, but in the process of evolution were absorbed by ancient microorganisms, archaea, and began to produce energy for them. Each cell can contain more than a thousand mitochondria, for example, the heart muscle cells have up to 5,000 mitochondria. Molecular motors, ATP synthase, embedded in the inner membrane of mitochondria, rotate under the influence of a stream of protons and synthesize the main source of energy - adenosine triphosphoric acid, ATP. It is estimated that the body of an adult synthesizes and consumes about 40 kg of ATP per day.
Mitochondria, unlike other organelles, have their own 2-10 copies of DNA, mtDNA. In the process of energy production, mitochondria generate toxic "waste" - reactive oxygen species (ROS), which can damage both other molecules and various cellular structures and, above all, mitochondria themselves, which can cause mutations in mitochondrial DNA and adversely affect the overall energy balance of the body. Thus, mtDNA deletions (precipitations) of mtDNA are able to multiply rapidly and fill the cellular space, causing sarcopenia and neurodegeneration. “Damaged” mitochondria begin to produce even larger amounts of ROS, leading to an increase in oxidative stress, which, in turn, can cause the development of various pathologies, premature aging and cell death.
An interesting fact related to oxidative stress. It was found that there is a clear correlation between the level of fatty acid saturation in membranes and the life expectancy of animals: the longer the membrane of unsaturated acids, the shorter the lifespan of the animal. Spanish biologists have traced such a sequence showing an increase in the life span while simultaneously decreasing the content of docosahexaenoic ω-3 fatty acid in the membranes: mouse → rat → rabbit → man → whale [1].
This pattern is easy to explain, because unsaturated fatty acids are the main "victims" of lipid peroxidation. Thus, the lipid composition of animal cell membranes, which is characterized by a longer life expectancy, demonstrates the golden mean: a small amount of completely unsaturated docosahexaenoic 22: 6 ω-3 fatty acids and the predominance of less unsaturated linolenic 18:03 ω-3 fatty acids, which it creates the same balance, providing both protection against ROS exposure and preserving the necessary fluidity of the membrane.
In addition to the lipid composition of animal cell membranes, the proportion of more thermodynamically stable guanine and cytosine among all mtDNA nucleotide residues also correlates with the maximum mammalian species lifetime [2].
The creators of the SENS concept see the solution to the problem of mitochondrial dysfunction in the transfer of "backup copies" of mitochondrial genes into the nucleus, where they cannot be damaged by ROS generated in mitochondria. Thus, even if the original genes in mtDNA are damaged, the backup copies in the nuclear DNA will be able to supply the proteins necessary to maintain normal energy production. This approach is called allotopic protein expression. Human mtDNA contains only 37 genes, of which only 13 encode proteins necessary for mitochondria, the rest (over 1000) of proteins coordinating the work of mitochondria are encoded in nuclear DNA. According to the authors of SENS, the transfer of the main mitochondrial genes into the nucleus was carried out by evolution precisely for this purpose - to protect them from the damaging action of ROS.
The idea of SENS authors about the evolutionary transfer of mitochondrial DNA into nuclear to protect mtDNA from harmful factors and, thus, prolong life, is confirmed in studies devoted to the analysis of the NUMT (nuclear mitochondrial DNA segment). The term NUMT refers to mtDNA fragments transferred to nuclear DNA. A comparative analysis of 17 species of animals with fully sequenced mitochondrial and nuclear genomes showed a significant positive correlation between life expectancy and the number of NUMT sequences [3]. It now remains to find an engineering solution for transferring backups of the remaining 13 mtDNA genes.
But there are alternative approaches to improving mitochondrial function. And one of them is transplantation of mitochondria from the outside. Successful “sharing” of alien mitochondria in experiments with animals has been described. Thus, mitochondrial transport was used in animal models for acute lung damage, cardiovascular diseases, and Parkinson's disease. Mitching of mitochondria can be accomplished in several ways: first, direct administration of isolated mitochondria (local administration), when isolated mitochondria are introduced directly into the cells of the damaged area; secondly, systemic administration, when the mitochondria are injected into the general circulation, and then they are distributed throughout the body. The results indicate the prospects for mitochondrial transplantation in the treatment of a number of diseases [4].
At the same time, it would be logical to find potential biomarkers for determining oxidative stress caused by mitochondrial dysfunction.
Oxidative stress is an imbalance between oxidants (active forms of oxygen) and antioxidant protection in the body towards oxidants. In cells, oxidants actively interact with biomolecules (phospholipids, proteins and nucleic acids). As a result, these biomolecules are irreversibly damaged, which leads to cellular dysfunction and, as a result, various pathologies in the body and cell death. One of the most popular theories of aging, free radical, proposed by D. Harman in the 1950s, sees this as the main mechanism of aging.
Molecules formed during oxidation can serve as biomarkers. Their analysis is used to quantify oxidative stress in humans. High concentrations of oxidative stress biomarkers are determined not only in age-related or degenerative diseases, such as Alzheimer's disease, hypertension, type 2 diabetes, or several types of cancer, but also in chronic obstructive pulmonary disease, smoking and living in ecologically unfavorable areas.
One of the most important biomarkers of oxidative stress is 8-iso prostaglandin F2α (8-isoprostane). 8-isoprostane is formed by non-enzymatic oxidation of phospholipids of cellular biomembranes, namely arachidonic acid. This prostaglandin-like substance causes constriction of blood vessels and bronchi, reduces blood flow in the kidneys, affects platelet aggregation and, thus, participates in the pathology of several diseases. Normal values of 8-isoprostane in healthy people are 11 ± 4 pg / ml [5].
Also recognized as a biomarker of lipid oxidation is malonic dialdehyde (MDA), which is formed during lipid peroxidation by free radicals and the breakdown of poly-saturated fatty acid molecules. The increased concentration of MDA in the serum serves as a marker not only of oxidative stress, but also the degree of endogenous intoxication. Therefore, an increase in the concentration of MDA in plasma is observed in smokers, as well as in people who abuse alcohol. MDA forms Schiff bases with amino groups of the protein, resulting in insoluble lipid-protein complexes (wear pigments or lipofuscin). MDA is determined in samples of many biological fluids: serum, plasma, urine, condensate of exhaled air. The concentration of MDA in the serum of healthy people (normal) is less than 1 µmol / l [6].
With the oxidation of amino acids that make up proteins, a number of potential biomarkers of oxidative stress are formed: o-tyrosine, 3-chlorothyrosine, and 3-nitrotyrosine.
Physiologically in the body, endogenous tyrosine is formed by the enzymatic oxidation of phenylalanine with phenylalanine hydroxylase. o-tyrosine (o-Tyr) and m-tyrosine (m-Tyr) are formed during the oxidation of phenylalanine with active forms of oxygen. o-Tyr and m-Tyr are not naturally occurring amino acids and are considered biomarkers of oxidative stress. High concentrations of o-Tyr and m-Tyr were found in patients with cataracts, and elevated o-Tyr was found in the blood plasma and urine of patients with type 2 diabetes. 3-Chlorothyrosine (3-ClTyr) is formed in free radical processes during the reaction of hypochlorous acid (HClO, a derivative of hydrogen peroxide) and p-tyrosine.
The formation of 3-ClTyr plays an important role in the cardiovascular system, since it is associated with the development of atherosclerosis. 3-ClTyr promotes the migration of smooth muscle cells of the human aorta (the main mechanism for the formation of vascular lesions), and elevated levels of 3-ClTyr in inflammatory conditions may contribute to vascular diseases. 3-nitrotyrosine (3-Notyr) is formed under oxidative stress by nitration of tyrosine with aggressive phagocytic protein myeloperoxidase (MPO). Such nitration adversely affects the function of the protein. Higher concentrations of 3-Notyr were found in the cerebrospinal fluid of Alzheimer's patients (11.4 ± 5.4 nM in patients and 1.6 ± 0.4 nM in the group of healthy volunteers), as well as in people with arthritis, atherosclerosis and hypertension [5].
Also, under the action of ROS and HClO on proteins, various oxidation products of proteins (AOPP) are formed. Such proteins do not perform their functions and can cause significant harm. AOPPs are produced by the myeloperoxidase-hydrogen peroxide system. Higher concentrations of AOPP have been detected in the plasma or urine of patients with acute coronary syndrome or active ulcerative colitis. Plasma levels of 60–70 nM are considered normal indicators of AORP in healthy people [5].
Well-known biomarkers of nucleic acid oxidation are 8-hydroxyguanosine (8-OHG) and 8-hydroxy-2'-deoxyguanosine (8-OHdG). 8-OHdG is the main product of DNA oxidation. 8-OHG is formed by the oxidation of RNA. A higher concentration of 8-OHdG is found in patients with Alzheimer's disease, arthritis, atherosclerosis, cataracts, hypertension, osteoporosis, and type 2 diabetes. 8-OHdG is also considered a potential biomarker for smoking-related cancer (for example, lung cancer). 8-OHG can be detected in Alzheimer's patients, and it has been shown that oxidative damage to RNA is higher than DNA damage. Blood concentrations of 8-OHdG in healthy people are 1.09 ± 0.52 nM, and levels of 8-OHG (in the cerebrospinal fluid) are 97 ± 32 pM [5].
Another biomarker that determines mitochondrial dysfunction and oxidative stress is the number of copies of cellular mtDNA (there is also extracellular mtDNA, which enters the blood during cell breakdown and its level increases with age). So, it is known that the number of cellular mtDNA decreases with age, and in men it is more than in women. A lower mtDNA count is also significantly associated with the development of senile asthenia (frailty). The number of copies of mtDNA can also be an effective prognostic marker for all-cause mortality, cardiovascular, cancer and respiratory diseases [7].
Endogenous antioxidants, such as glutathione, cysteine, uric acid and ubiquinol, also have potential for use as biomarkers of mitochondrial dysfunction and oxidative stress. When interacting with active forms of oxygen, endogenous antioxidants are oxidized, but then restored again with the help of special enzymes. Therefore, in the body, antioxidant molecules are present in two forms: reduced form (antioxidant) or oxidized (after reaction with oxidants). Using the chromatographic method, it is possible to record the ratio of reduced and oxidized forms of antioxidants and thus determine the degree of oxidative stress [8].
Biomarkers of mitochondrial dysfunction and oxidative stress:
1. 8-isoprostane.
2. Malonic dialdehyde
3. O-tyrosine, 3-chlorothyrosine, 3-nitrotyrosine.
4. Protein Oxidation Products (AOPP).
5. 8-hydroxyguanosine (8-OHG)
6. 8-hydroxy-2'-deoxyguanosine (8-OHdG).
7. Cellular mtDNA (its number and the presence of mutated variants with deletions)
8. Endogenous antioxidants (glutathione, cysteine, uric acid, ubiquinol).
Review authors: Denis Odinokov, Alexey Rzheshevsky.
References:
1. Pamplona, R., Portero_Otnn, M., Ruiz, C., Gredilla, R., Herrero, A., and Barja, G. (2000) peroxidation is negatively correlated with the lithium peroxidation heart of mammals, mech. Aging Dev., 112, 169-183.
2. Lehmann G1, Segal E, Muradian KK, Fraifeld VE. Do you want to have a mammalian maximum longevity? Rejuvenation Res. 2008 Apr; 11 (2): 409-17.
3. Muradian KK1, Lehmann G, Fraifeld VE. NUMT ("new mighty") hypothesis of longevity. Rejuvenation Res. 2010 Apr-Jun; 13 (2-3): 152-5.
4. Gollihue, Jenna L., Samir P. Patel, and Alexander G. Rabchevsky. Mitochondrial transplantation strategies for the central nervous system trauma. Neural regeneration research13.2 (2018): 194.
5. Kamila Syslová, Adéla Böhmová, Miloš Mikoška, Marek Kuzma, Daniela Pelclová, and Petr Kačer. Multimarker screening of oxidative stress in aging. Oxid Med Cell Longev. 2014; 562860. Published online 2014 Jul 16.
6. Yashin A., Yashin Ya. High-performance liquid chromatography of markers of oxidative stress. 2011. Analytics. No. 1, 34-43.
7. Foram N. et al. Association of Mitochondrial DNA levels with Frailty and All-Cause Mortality. J Mol Med (Berl). 2015 Feb; 93 (2): 177–186.
8. Zhloba A.A. Subbotina T.F., Alekseevskaya E.S., Moiseeva OM., Gavrilyuk N.D., Irtyuga O.B. Metabolic and protein markers of mitochondrial dysfunction in patients with cardiovascular diseases. Clinical laboratory diagnostics. 2015; 60 (7): 35–41.
2. Lehmann G1, Segal E, Muradian KK, Fraifeld VE. Do you want to have a mammalian maximum longevity? Rejuvenation Res. 2008 Apr; 11 (2): 409-17.
3. Muradian KK1, Lehmann G, Fraifeld VE. NUMT ("new mighty") hypothesis of longevity. Rejuvenation Res. 2010 Apr-Jun; 13 (2-3): 152-5.
4. Gollihue, Jenna L., Samir P. Patel, and Alexander G. Rabchevsky. Mitochondrial transplantation strategies for the central nervous system trauma. Neural regeneration research13.2 (2018): 194.
5. Kamila Syslová, Adéla Böhmová, Miloš Mikoška, Marek Kuzma, Daniela Pelclová, and Petr Kačer. Multimarker screening of oxidative stress in aging. Oxid Med Cell Longev. 2014; 562860. Published online 2014 Jul 16.
6. Yashin A., Yashin Ya. High-performance liquid chromatography of markers of oxidative stress. 2011. Analytics. No. 1, 34-43.
7. Foram N. et al. Association of Mitochondrial DNA levels with Frailty and All-Cause Mortality. J Mol Med (Berl). 2015 Feb; 93 (2): 177–186.
8. Zhloba A.A. Subbotina T.F., Alekseevskaya E.S., Moiseeva OM., Gavrilyuk N.D., Irtyuga O.B. Metabolic and protein markers of mitochondrial dysfunction in patients with cardiovascular diseases. Clinical laboratory diagnostics. 2015; 60 (7): 35–41.
Source: https://habr.com/ru/post/421225/
All Articles