What a disease: diabetes
Everyone has their own ideas about diabetes. Someone thinks that it starts if you eat thirty chocolates in a row, although this is not so. For someone, diabetes is an "innocuous" chronic disease. But according to statistics from the World Health Organization, 1.5 million people die from diabetes mellitus per year - more than from human immunodeficiency virus.
Today , Atlas talks about how diabetes is, why it occurs, and how to manage the risks of developing the disease.
')
To understand the mechanism of diabetes, you need to know the principles of carbohydrate metabolism. This is a complex metabolic process, in which the body receives and consumes energy.
For normal operation, cells need energy, the main source of which is carbohydrates. They are found in most foods that people eat.
In the intestine, carbohydrates are broken down into simple compounds (monosaccharides), absorbed into the mucous membrane and enter the blood. The body is always ready to respond to glucose abnormalities. He is assisted in this by some receptors and signaling molecules — peptides, which the stomach secretes. In a healthy body, this reaction happens very quickly.
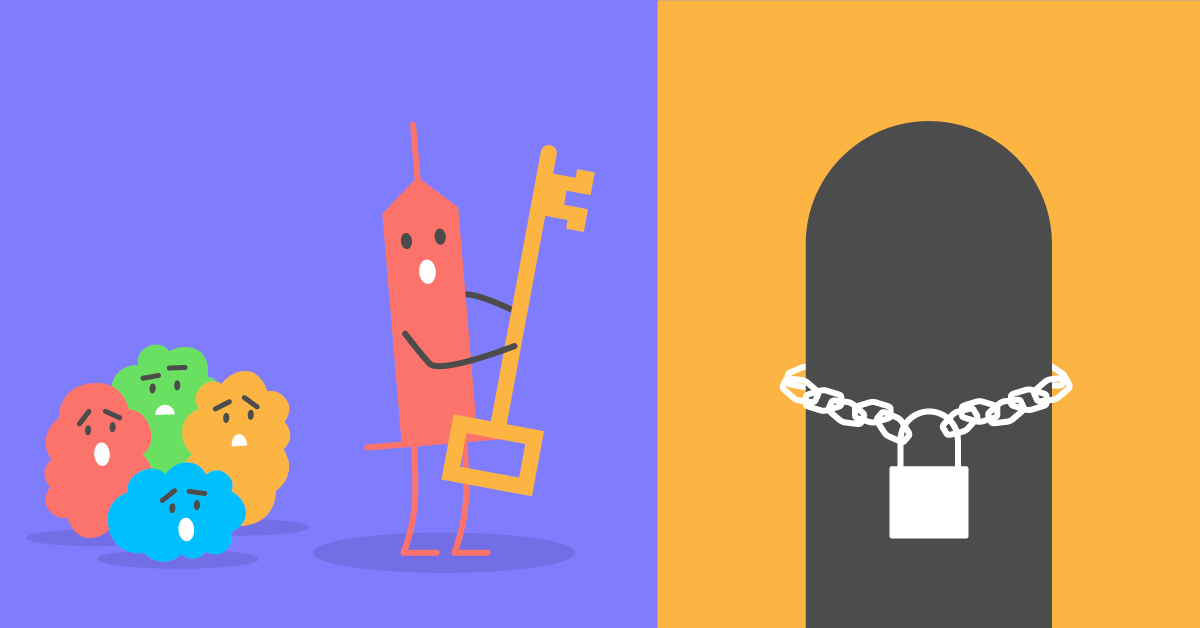
Glucose cannot get into the cells by itself: to avoid the uncontrolled movement of glucose, the cell closes its doors to the lock. In the role of a locking device are the receptors of the GLUT family - proteins on the surface of the cell membrane. Some of them open automatically, but most need a key - a special hormone insulin.
The exception is the brain cells: this is too important an organ to give its energy supply “to outsource”. Therefore, “locks” —GLUT receptors in brain cells open automatically without the participation of insulin. The concentration of glucose in the blood is equalized with the concentration in neurons. That is why, when we are hungry, we are so eager to eat something sweet and immediately supply the brain cells with energy.

Insulin produces pancreatic beta cells located in the islets of Langerhans. From the name of these cells Insulae pancreaticae and the name of insulin. Beta cells react to an increase in the level of glucose in the blood, as well as to the signal peptides of the APUP-system, which are released when food gets into the stomach, long before the increase in glucose.
In response to these signals, the beta cells of the islets of Langerhans activate insulin production. The hormone enters the bloodstream, bypasses the cells of the body, opens the locks - and the cells get the necessary energy.
But the story does not end there. What if the body got more energy than its cells need? And what to do after a meal when glucose levels fall? Evolution has a simple answer to these questions: food is not every day, and all that can be put off is needed to be put off.
There are several storages of energy in the body: say, a refrigerator where you can leave food for a couple of days, and a cellar where food is stored for the winter.
The refrigerator, or the nearest storage, is glycogen storage. While glucose bypasses the cells, in the liver its excess is packed into glycogen. This process is called glycogenogenesis. Packaging requires energy, but unpacking does not. Therefore, glycogen is convenient to use to maintain energy when the level of glucose in the blood decreases. This happens a few hours after eating.
The hormone glucagon is released in the absence of insulin and helps to decompress glycogens and decompose to a simple glucose state. This process is called glycogenolysis, it occurs in the liver and in the muscles. From the liver, glucose is transported into the blood and can then be used in different tissues. In muscles, unpacked glucose is consumed immediately and is not transported anywhere.

The “refrigerator” is not rubber, and when glycogen stores are created, and glucose is still circulating in the blood, the body stores up unused glucose as fat. In the liver, carbohydrates are transformed into fatty acids. Then glycerol is added to them, the molecules are converted into triglycerides and sent to storage in adipose tissue.
Triglycerides and fatty acids can be ingested with food, as part of fatty foods. Some of them are transported to the liver and then to the blood; another part of the lymphatic system is sent immediately to the adipose tissue. Cells can use fatty acids as an energy source or send to storage in adipose tissue.
To transform fat molecules into glucose, the body spends a lot of energy. Therefore, he resorts to such measures only after all other sources of energy, both glucose and glycogen, have been consumed. The process of recovering glucose from non-carbohydrate elements is called gluconeogenesis.
Metabolic processes in the body allow you to adjust the level of glucose and maintain energy at the right level, not only during meals, but also on an empty stomach. As is often the case with complex cascade reactions, failure of one element leads to an imbalance of the entire system.
Type 1 diabetes mellitus (type 1 diabetes) accounts for 10% of all diabetes mellitus cases. It is also called "child". Despite the fact that a quarter of cases are adults, this variant of diabetes is more often seen in children and adolescents.
Type 1 diabetes mellitus is a chronic disease, most often due to autoimmune disorders. For reasons unknown to the end, the body begins to attack the beta cells of the islets of Langerhans. Any external stressful event can be a trigger: the beta cells have an imperfect antigens complex, and the immune system can consider them a tumor and start an attack.
Destroyed beta cells stop producing insulin. Now there is no one to open the "locks" of cells, they do not receive energy, and tissue starvation begins. The body "unpacks" the reserves of fat at a rate for which the metabolic processes are not calculated. There are too many toxic ketone bodies in the blood that acidify the blood and cause ketoacidosis. This is a metabolic disease in which the acid balance in the body shifts. Ketoacidosis is the main reason why patients with type 1 diabetes are in the hospital.
Among the possible factors influencing the risk of T1DM - genetic predisposition and infection. This is a rare disease, and even the presence of a genetic predisposition does not significantly affect its risk. Among the infectious diseases associated with type 1 diabetes, the Coxsackie virus, Epstein-Barr virus, and cytomegalovirus are noted. These viruses can destroy the beta cells of the islets of Langerhans or provoke an autoimmune attack on them. There is no connection between vaccines and the risk of type 1 diabetes.
Symptoms of type 1 diabetes: loss of appetite and weight, abundant thirst and urination, constant fatigue. SD1 develops quite quickly. The onset of the disease can coincide with stressful situations - infections, surgery. Often the patient learns about the disease in the emergency room after the loss of consciousness as a result of ketoacidosis. Therefore, it is important for parents to remember that strong thirst and frequent urination in a child is a reason to consult a doctor without delay.
A treatment for type 1 diabetes has not yet been found, but there are tools for controlling glucose levels. To do this, patients constantly measure blood glucose levels and inject insulin. There were attempts to transplant the pancreas, but such operations did not show sufficient effectiveness.
Automated tools are being developed that will maintain normal glucose levels. Last year, the FDA approved an artificial pancreas. This is an external wearable device that consists of an insulin pump and a sensor. The algorithm calculates the dose and automatically injects the right amount of insulin.
There are no effective methods for preventing T1DM - and this is its difference with type 2 diabetes.
Type 2 diabetes mellitus (DM2) is a multifactorial disease, in the development of which both genetic factors and lifestyle play a role. It accounts for 90% of diabetes cases.
T2DM develops due to the low sensitivity of cells to insulin, against the background of which the normal amount of insulin becomes insufficient. If diabetes mellitus type 1 begins after the death of beta cells, then with diabetes mellitus type 2, the islet cells of Largengans continue to function (at least at the time of the manifestation). They continue to produce insulin, which also goes to the cells, in front of which crowds of glucose have accumulated - but the trouble is, the castle is covered up with some kind of filth. The key — the receptor does not work, and glucose cannot enter the cell.
The causes of type 2 diabetes are genetic predisposition multiplied by overweight and low active lifestyle. At the same time, obesity does not trigger the disease itself, but only when superimposed on negative hereditary factors. In the absence of genetic predisposition, overweight may not lead to type 2 diabetes (which does not exclude cardiovascular complications). But among overweight people, only 6.8–36.6% have no metabolic disturbances and a tendency to insulin resistance.
The classic symptoms of type 2 diabetes are similar to type 1 diabetes - the same chronic fatigue, profuse thirst and urination, weight loss while maintaining a lifestyle. Diagnosis at a stage when the disease has already manifested itself in the form of symptoms, is considered late. There are earlier symptoms: a problem with the gums and teeth, pustular rash, frequent diseases of the urinary tract. If there are similar manifestations, you need to pass the analysis for glycated hemoglobin.
At the stage of timely diagnosis, diabetes mellitus type 2 has no symptoms. SD2 can develop over the years and go unnoticed. In order to detect the signs of diabetes mellitus as early as possible, special questionnaires need to be filled out, and after 40 years of age - to undergo an annual screening examination.
Prophylactic screening is recommended for people who have overweight combined with one of the following factors:
Unlike type 1 diabetes, the risk of T2DM can be managed. Proper nutrition, normal weight and at least 150 minutes of exercise per week (cardio and aerobic exercise) reduce the risk of type 2 diabetes even with genetic prerequisites. Strength and weightlifting do not affect the risk of T2DM, although such exercises are especially good for people with a predisposition to diabetes.
Type 2 diabetes cannot be completely cured, you can only slow down its development and control complications. In the early stages it is enough to change lifestyle and take pills. They increase insulin sensitivity and compensate for genetic factors.
If you lose weight to normal BMI, insulin sensitivity of the tissues can be restored, and blood glucose will be maintained at a normal level. In this case, patients are still advised to take pills to help their own insulin remain effective.
Diabetes mellitus type 1 and 2 has three types of complications. Neuropathic disorders occur due to sudden changes in sugar levels. Microvascular complications include kidney and retinal damage due to persistently high sugar levels. Macrovascular diseases are affected by cholesterol levels and the mere presence of diabetes.
Diabetes mellitus is associated with a high risk of atherosclerosis. Constantly elevated blood sugar levels cause systemic inflammation, which leads to the deposition of cholesterol in the walls of blood vessels and their narrowing. With the growth of plaques a thrombus can form and block the blood flow.
Diabetes mellitus type 2 is accompanied by an increase in blood pressure, since insulin stimulates the reabsorption of sodium in the kidneys. This causes water retention and increased blood volume. This is the most significant risk factor for strokes and heart attacks. We will describe how to properly control blood pressure in another article.
Another complication of diabetes is diabetic foot syndrome. It occurs for two reasons: due to the defeat of the peripheral nerves or blockage of blood vessels in atherosclerosis. In the first case, the sensitivity and nutrition of the skin of the feet decreases, ulcers appear. As a rule, they do not hurt and can go unnoticed for a long time. In such a situation, unloading of the foot and the treatment of wounds helps.
When blood vessels are blocked, the blood supply to the foot is disrupted - this is a potentially more dangerous case. Delay in treatment can lead to tissue necrosis and, in severe cases, to leg amputation. Therefore, if blood supply is disturbed and pain appears, you should immediately consult a doctor and restore blood flow. If this is not done within 24 hours, the leg will no longer be saved.
To avoid such consequences, you need to carefully follow the rules of prevention and respond to changes in time.
The risk of developing diabetes is affected by a complex of about a hundred genes. They are at different levels associated with the work of insulin, from synthesis to transportation and the structure of the receptors. Here we will tell only about some of them.
Insulin receptors encode genes for the GLUT family. Different types of receptors are found in different cells: GLUT1 delivers glucose to the erythrocytes, GLUT2 to the liver and pancreas, GLUT3 to the nervous tissue and placenta, GLUT4 to the fat and muscle tissue and to the myocardial cells (heart muscles). Mutations in these genes lead to insulin resistance.
The TCF7L2 gene determines the work of the signaling pathways, it affects the synthesis and secretion of insulin and proglucagon, the protein precursor of glucagon. Mutations in the gene lead to a decrease in insulin production in the body. The GCGR gene encodes the glucagon receptor protein, a hormone that, together with insulin, helps regulate blood glucose levels.
Since obesity increases the risk of T2DM, genes that affect eating behavior are associated with the disease. For example, the FTO gene is Fat Mass And Obesity Associated. His work is associated with a feeling of saturation. In people with a specific variant of the FTO gene, the feeling of satiety comes with a delay of 10-15 minutes. During this time, you can have time to eat too much. Therefore, people with this type of gene have a potentially higher risk of obesity and type 2 diabetes.
Obesity, type 2 diabetes, insulin resistance - all of these diseases are associated with chronic inflammation. Some of these processes take place in the intestines and depend on the composition of the community of intestinal bacteria.
In the intestines live different types of bacteria, all together they are called microbiota. Each type of bacteria has its own tasks. Some bacteria, mainly from the class of clostridia, produce butyric acid. It is a useful substance that nourishes the intestinal wall and protects against inflammation. For the synthesis of butyric acid bacteria need fiber. In patients with type 2 diabetes, the level of butyric acid-producing bacteria is reduced, and inflammation begins in the intestine.
In T2DM, the microbiota lacks another bacterium, Akkermansia muciniphila . The presence of bacteria of this species in the intestines is an indicator of a healthy metabolism. The akkermansiya mutsinifila often occurs in people with normal weight, but with obesity, its number decreases sharply.
According to the composition of the microbiota, it is possible to see in advance the changes in the intestinal bacterial community characteristic of inflammation and to begin prevention: first of all, change the diet. You need to add more high fiber foods to your diet to support intestinal bacteria that protect against inflammation.
Type 1 diabetes is rare, and, unfortunately, its development cannot be prevented. But the risk of developing type 2 diabetes can be controlled. To do this, you need to follow the weight, especially with a genetic predisposition, to maintain an active lifestyle, choose the right diet.
It is not enough to count the number of calories received and consumed per day. It is necessary to monitor the balance of nutrients in food and give preference to complex carbohydrates and fiber.
The hereditary risks of type 2 diabetes will help determine the Atlas genetic test . The role of intestinal bacteria and their contribution to the protection of the body against the disease will be evaluated by the test “Genetics of microbiota” . If you have a predisposition for diabetes mellitus, or a relative with such a disease - contact an endocrinologist to make an individual prevention plan.
Today , Atlas talks about how diabetes is, why it occurs, and how to manage the risks of developing the disease.
')
To understand the mechanism of diabetes, you need to know the principles of carbohydrate metabolism. This is a complex metabolic process, in which the body receives and consumes energy.
Glucose - a source of energy in the body
For normal operation, cells need energy, the main source of which is carbohydrates. They are found in most foods that people eat.
In the intestine, carbohydrates are broken down into simple compounds (monosaccharides), absorbed into the mucous membrane and enter the blood. The body is always ready to respond to glucose abnormalities. He is assisted in this by some receptors and signaling molecules — peptides, which the stomach secretes. In a healthy body, this reaction happens very quickly.
Glucose cannot get into the cells by itself: to avoid the uncontrolled movement of glucose, the cell closes its doors to the lock. In the role of a locking device are the receptors of the GLUT family - proteins on the surface of the cell membrane. Some of them open automatically, but most need a key - a special hormone insulin.
The exception is the brain cells: this is too important an organ to give its energy supply “to outsource”. Therefore, “locks” —GLUT receptors in brain cells open automatically without the participation of insulin. The concentration of glucose in the blood is equalized with the concentration in neurons. That is why, when we are hungry, we are so eager to eat something sweet and immediately supply the brain cells with energy.

Insulin triggers glucose into the cell.
Insulin produces pancreatic beta cells located in the islets of Langerhans. From the name of these cells Insulae pancreaticae and the name of insulin. Beta cells react to an increase in the level of glucose in the blood, as well as to the signal peptides of the APUP-system, which are released when food gets into the stomach, long before the increase in glucose.
In response to these signals, the beta cells of the islets of Langerhans activate insulin production. The hormone enters the bloodstream, bypasses the cells of the body, opens the locks - and the cells get the necessary energy.
But the story does not end there. What if the body got more energy than its cells need? And what to do after a meal when glucose levels fall? Evolution has a simple answer to these questions: food is not every day, and all that can be put off is needed to be put off.
Glycogen and triglycerides - glucose storage
There are several storages of energy in the body: say, a refrigerator where you can leave food for a couple of days, and a cellar where food is stored for the winter.
The refrigerator, or the nearest storage, is glycogen storage. While glucose bypasses the cells, in the liver its excess is packed into glycogen. This process is called glycogenogenesis. Packaging requires energy, but unpacking does not. Therefore, glycogen is convenient to use to maintain energy when the level of glucose in the blood decreases. This happens a few hours after eating.
The hormone glucagon is released in the absence of insulin and helps to decompress glycogens and decompose to a simple glucose state. This process is called glycogenolysis, it occurs in the liver and in the muscles. From the liver, glucose is transported into the blood and can then be used in different tissues. In muscles, unpacked glucose is consumed immediately and is not transported anywhere.

The “refrigerator” is not rubber, and when glycogen stores are created, and glucose is still circulating in the blood, the body stores up unused glucose as fat. In the liver, carbohydrates are transformed into fatty acids. Then glycerol is added to them, the molecules are converted into triglycerides and sent to storage in adipose tissue.
Triglycerides and fatty acids can be ingested with food, as part of fatty foods. Some of them are transported to the liver and then to the blood; another part of the lymphatic system is sent immediately to the adipose tissue. Cells can use fatty acids as an energy source or send to storage in adipose tissue.
To transform fat molecules into glucose, the body spends a lot of energy. Therefore, he resorts to such measures only after all other sources of energy, both glucose and glycogen, have been consumed. The process of recovering glucose from non-carbohydrate elements is called gluconeogenesis.
Metabolic processes in the body allow you to adjust the level of glucose and maintain energy at the right level, not only during meals, but also on an empty stomach. As is often the case with complex cascade reactions, failure of one element leads to an imbalance of the entire system.
Type 1 diabetes mellitus - lack of insulin
Type 1 diabetes mellitus (type 1 diabetes) accounts for 10% of all diabetes mellitus cases. It is also called "child". Despite the fact that a quarter of cases are adults, this variant of diabetes is more often seen in children and adolescents.
Type 1 diabetes mellitus is a chronic disease, most often due to autoimmune disorders. For reasons unknown to the end, the body begins to attack the beta cells of the islets of Langerhans. Any external stressful event can be a trigger: the beta cells have an imperfect antigens complex, and the immune system can consider them a tumor and start an attack.
Destroyed beta cells stop producing insulin. Now there is no one to open the "locks" of cells, they do not receive energy, and tissue starvation begins. The body "unpacks" the reserves of fat at a rate for which the metabolic processes are not calculated. There are too many toxic ketone bodies in the blood that acidify the blood and cause ketoacidosis. This is a metabolic disease in which the acid balance in the body shifts. Ketoacidosis is the main reason why patients with type 1 diabetes are in the hospital.
Among the possible factors influencing the risk of T1DM - genetic predisposition and infection. This is a rare disease, and even the presence of a genetic predisposition does not significantly affect its risk. Among the infectious diseases associated with type 1 diabetes, the Coxsackie virus, Epstein-Barr virus, and cytomegalovirus are noted. These viruses can destroy the beta cells of the islets of Langerhans or provoke an autoimmune attack on them. There is no connection between vaccines and the risk of type 1 diabetes.
Symptoms of type 1 diabetes: loss of appetite and weight, abundant thirst and urination, constant fatigue. SD1 develops quite quickly. The onset of the disease can coincide with stressful situations - infections, surgery. Often the patient learns about the disease in the emergency room after the loss of consciousness as a result of ketoacidosis. Therefore, it is important for parents to remember that strong thirst and frequent urination in a child is a reason to consult a doctor without delay.
A treatment for type 1 diabetes has not yet been found, but there are tools for controlling glucose levels. To do this, patients constantly measure blood glucose levels and inject insulin. There were attempts to transplant the pancreas, but such operations did not show sufficient effectiveness.
Automated tools are being developed that will maintain normal glucose levels. Last year, the FDA approved an artificial pancreas. This is an external wearable device that consists of an insulin pump and a sensor. The algorithm calculates the dose and automatically injects the right amount of insulin.
There are no effective methods for preventing T1DM - and this is its difference with type 2 diabetes.
Type 2 Diabetes - Insulin Helplessness
Type 2 diabetes mellitus (DM2) is a multifactorial disease, in the development of which both genetic factors and lifestyle play a role. It accounts for 90% of diabetes cases.
T2DM develops due to the low sensitivity of cells to insulin, against the background of which the normal amount of insulin becomes insufficient. If diabetes mellitus type 1 begins after the death of beta cells, then with diabetes mellitus type 2, the islet cells of Largengans continue to function (at least at the time of the manifestation). They continue to produce insulin, which also goes to the cells, in front of which crowds of glucose have accumulated - but the trouble is, the castle is covered up with some kind of filth. The key — the receptor does not work, and glucose cannot enter the cell.
The causes of type 2 diabetes are genetic predisposition multiplied by overweight and low active lifestyle. At the same time, obesity does not trigger the disease itself, but only when superimposed on negative hereditary factors. In the absence of genetic predisposition, overweight may not lead to type 2 diabetes (which does not exclude cardiovascular complications). But among overweight people, only 6.8–36.6% have no metabolic disturbances and a tendency to insulin resistance.
The classic symptoms of type 2 diabetes are similar to type 1 diabetes - the same chronic fatigue, profuse thirst and urination, weight loss while maintaining a lifestyle. Diagnosis at a stage when the disease has already manifested itself in the form of symptoms, is considered late. There are earlier symptoms: a problem with the gums and teeth, pustular rash, frequent diseases of the urinary tract. If there are similar manifestations, you need to pass the analysis for glycated hemoglobin.
At the stage of timely diagnosis, diabetes mellitus type 2 has no symptoms. SD2 can develop over the years and go unnoticed. In order to detect the signs of diabetes mellitus as early as possible, special questionnaires need to be filled out, and after 40 years of age - to undergo an annual screening examination.
Prophylactic screening is recommended for people who have overweight combined with one of the following factors:
- The diagnosis of type 2 diabetes in a relative;
- Cardiovascular disease in the history of the disease;
- Elevated blood cholesterol;
- High blood pressure;
- Sedentary lifestyle;
- The birth of a large child (more than 3600 g).
Unlike type 1 diabetes, the risk of T2DM can be managed. Proper nutrition, normal weight and at least 150 minutes of exercise per week (cardio and aerobic exercise) reduce the risk of type 2 diabetes even with genetic prerequisites. Strength and weightlifting do not affect the risk of T2DM, although such exercises are especially good for people with a predisposition to diabetes.
Type 2 diabetes cannot be completely cured, you can only slow down its development and control complications. In the early stages it is enough to change lifestyle and take pills. They increase insulin sensitivity and compensate for genetic factors.
If you lose weight to normal BMI, insulin sensitivity of the tissues can be restored, and blood glucose will be maintained at a normal level. In this case, patients are still advised to take pills to help their own insulin remain effective.
Diabetes leads to severe complications
Diabetes mellitus type 1 and 2 has three types of complications. Neuropathic disorders occur due to sudden changes in sugar levels. Microvascular complications include kidney and retinal damage due to persistently high sugar levels. Macrovascular diseases are affected by cholesterol levels and the mere presence of diabetes.
Diabetes mellitus is associated with a high risk of atherosclerosis. Constantly elevated blood sugar levels cause systemic inflammation, which leads to the deposition of cholesterol in the walls of blood vessels and their narrowing. With the growth of plaques a thrombus can form and block the blood flow.
Diabetes mellitus type 2 is accompanied by an increase in blood pressure, since insulin stimulates the reabsorption of sodium in the kidneys. This causes water retention and increased blood volume. This is the most significant risk factor for strokes and heart attacks. We will describe how to properly control blood pressure in another article.
Another complication of diabetes is diabetic foot syndrome. It occurs for two reasons: due to the defeat of the peripheral nerves or blockage of blood vessels in atherosclerosis. In the first case, the sensitivity and nutrition of the skin of the feet decreases, ulcers appear. As a rule, they do not hurt and can go unnoticed for a long time. In such a situation, unloading of the foot and the treatment of wounds helps.
When blood vessels are blocked, the blood supply to the foot is disrupted - this is a potentially more dangerous case. Delay in treatment can lead to tissue necrosis and, in severe cases, to leg amputation. Therefore, if blood supply is disturbed and pain appears, you should immediately consult a doctor and restore blood flow. If this is not done within 24 hours, the leg will no longer be saved.
To avoid such consequences, you need to carefully follow the rules of prevention and respond to changes in time.
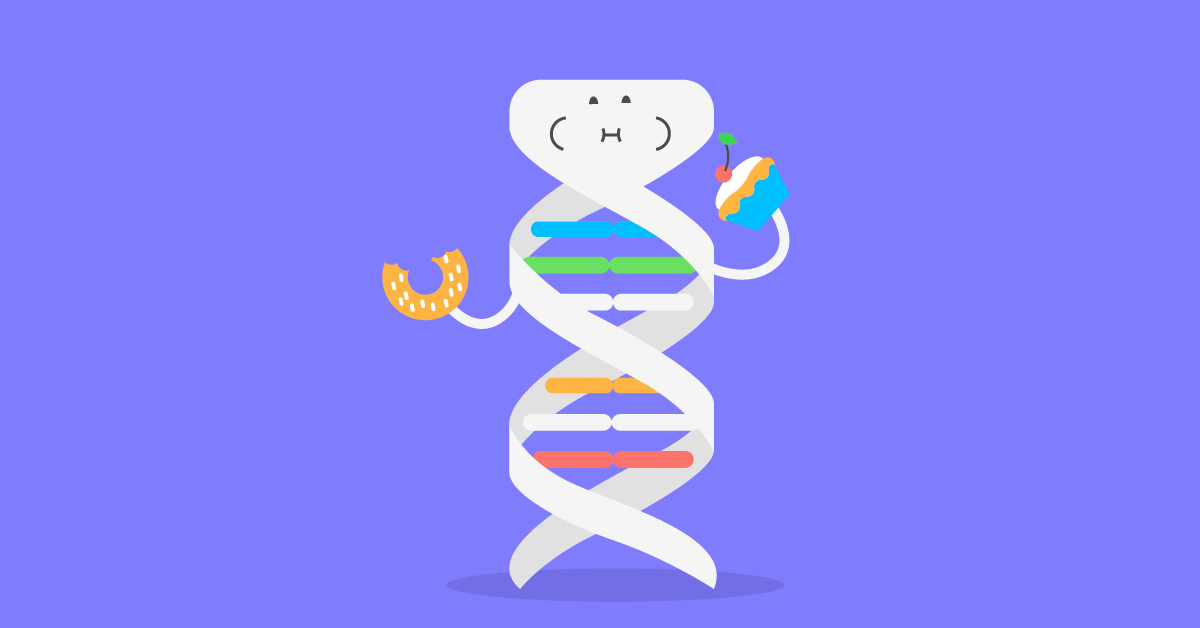
Genetics affects the risk of developing type 2 diabetes
The risk of developing diabetes is affected by a complex of about a hundred genes. They are at different levels associated with the work of insulin, from synthesis to transportation and the structure of the receptors. Here we will tell only about some of them.
Insulin receptors encode genes for the GLUT family. Different types of receptors are found in different cells: GLUT1 delivers glucose to the erythrocytes, GLUT2 to the liver and pancreas, GLUT3 to the nervous tissue and placenta, GLUT4 to the fat and muscle tissue and to the myocardial cells (heart muscles). Mutations in these genes lead to insulin resistance.
The TCF7L2 gene determines the work of the signaling pathways, it affects the synthesis and secretion of insulin and proglucagon, the protein precursor of glucagon. Mutations in the gene lead to a decrease in insulin production in the body. The GCGR gene encodes the glucagon receptor protein, a hormone that, together with insulin, helps regulate blood glucose levels.
Since obesity increases the risk of T2DM, genes that affect eating behavior are associated with the disease. For example, the FTO gene is Fat Mass And Obesity Associated. His work is associated with a feeling of saturation. In people with a specific variant of the FTO gene, the feeling of satiety comes with a delay of 10-15 minutes. During this time, you can have time to eat too much. Therefore, people with this type of gene have a potentially higher risk of obesity and type 2 diabetes.
In type 2 diabetes, the composition of the microbiota changes
Obesity, type 2 diabetes, insulin resistance - all of these diseases are associated with chronic inflammation. Some of these processes take place in the intestines and depend on the composition of the community of intestinal bacteria.
In the intestines live different types of bacteria, all together they are called microbiota. Each type of bacteria has its own tasks. Some bacteria, mainly from the class of clostridia, produce butyric acid. It is a useful substance that nourishes the intestinal wall and protects against inflammation. For the synthesis of butyric acid bacteria need fiber. In patients with type 2 diabetes, the level of butyric acid-producing bacteria is reduced, and inflammation begins in the intestine.
In T2DM, the microbiota lacks another bacterium, Akkermansia muciniphila . The presence of bacteria of this species in the intestines is an indicator of a healthy metabolism. The akkermansiya mutsinifila often occurs in people with normal weight, but with obesity, its number decreases sharply.
According to the composition of the microbiota, it is possible to see in advance the changes in the intestinal bacterial community characteristic of inflammation and to begin prevention: first of all, change the diet. You need to add more high fiber foods to your diet to support intestinal bacteria that protect against inflammation.
The risks of type 2 diabetes can be managed
Type 1 diabetes is rare, and, unfortunately, its development cannot be prevented. But the risk of developing type 2 diabetes can be controlled. To do this, you need to follow the weight, especially with a genetic predisposition, to maintain an active lifestyle, choose the right diet.
It is not enough to count the number of calories received and consumed per day. It is necessary to monitor the balance of nutrients in food and give preference to complex carbohydrates and fiber.
The hereditary risks of type 2 diabetes will help determine the Atlas genetic test . The role of intestinal bacteria and their contribution to the protection of the body against the disease will be evaluated by the test “Genetics of microbiota” . If you have a predisposition for diabetes mellitus, or a relative with such a disease - contact an endocrinologist to make an individual prevention plan.
Source: https://habr.com/ru/post/403347/
All Articles