How to treat crazy. 1.1 - Pharmacotherapy: Basics and Schizophrenia
Greetings,% username%!
This article is a logical continuation of the post devoted to pathopsychological diagnosis. In it, I will try to speak in an accessible language about the main groups of pharmacological drugs used to treat mental diseases, as well as about the mechanisms, structures and components of the human brain that are involved in this process.
')
Disclaimer : I am not a psychiatrist, but a psycho. I tested the drugs of all these groups on myself and watched their actions (when I was in an insane asylum). In addition, I have some experience in selecting pharmacy, but I do not have a formal education in this area. In this regard, as well as the fact that making a diagnosis according to scientific articles is an extremely wrong thing in its basis, I want to warn the reader that, before accepting any of the things described here, you must consult with a specialist. If real welders come to the post and substantiate the incorrectness of the stated theses, I will be only glad.
If the above does not scare you, I suggest to plunge into the fascinating world of psychopharmacology. In the post a lot of letters and pictures, I warn you immediately.
Before talking about the pharmacological methods of treating mental illness, it is necessary to consider some aspects of the structure and functioning of the human brain - just so that further material is clear.
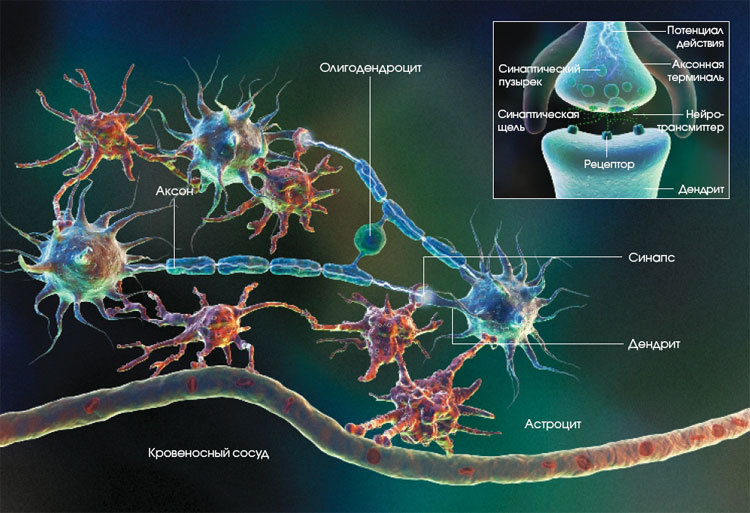
Most likely, everyone present knows that the brain consists of neurons and neuroglia (special cells that perform a variety of functions - trophic, structural, secretory, regulatory and protective [1, 3]) - the first are the main objects of our interest, the second is not so important for this article, since most modern pharmacology has no significant effect on it (more precisely, it has only in the context of side effects).
Neurons look like this:
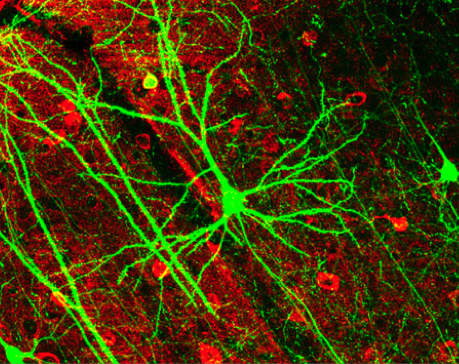
And glial cells - like this:
Contrary to popular belief, glial cells are quite involved in the transmission of nerve impulses [1], at least indirectly - by influencing the formation of synapses (about them - below), but all the drugs we know do not affect its cells and functions, but neurons and communication between them [4].
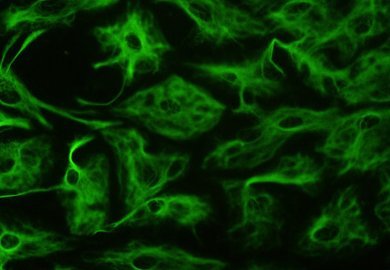
Consider an approximate model of the structure of the neuron:
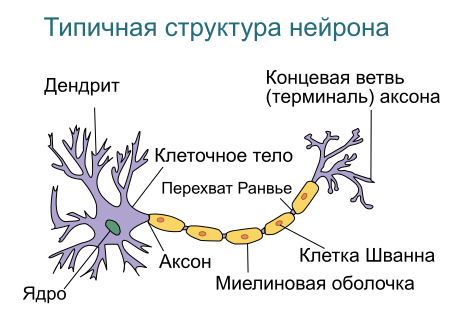
We are interested in dendrites - processes, through which a neuron receives messages from its fellows [6] (roughly speaking, the input of a neuron) and an axon - a process through which a neuron transmits its message (ie its “output”) [6].
Why is that? Because they are directly related to the signals that the neurons transmit to each other, and in these signals the whole “spiritual life” of a person (well, almost all) is encrypted: his thoughts, memories, beliefs, preferences, etc., including Of course, what is considered a manifestation of mental illness is delusional concepts, hallucinations, and so on [4].
Thus, the task of treating mental diseases is reduced (within the framework of the biologizing approach , namely, it is the basis of this article, we will talk about others separately) to the task of changing the parameters of the passage of signals between neurons and those events that occur in the neurons themselves due to this transfer [4]. Of course, not an arbitrary change, but a directed and controlled one.
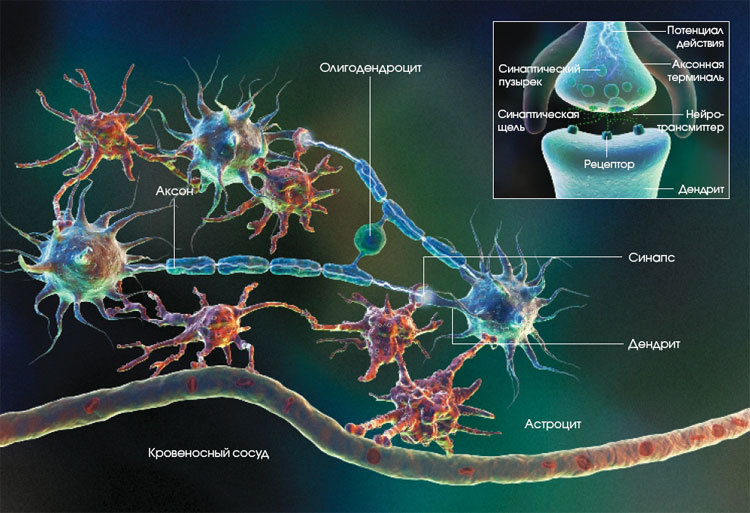
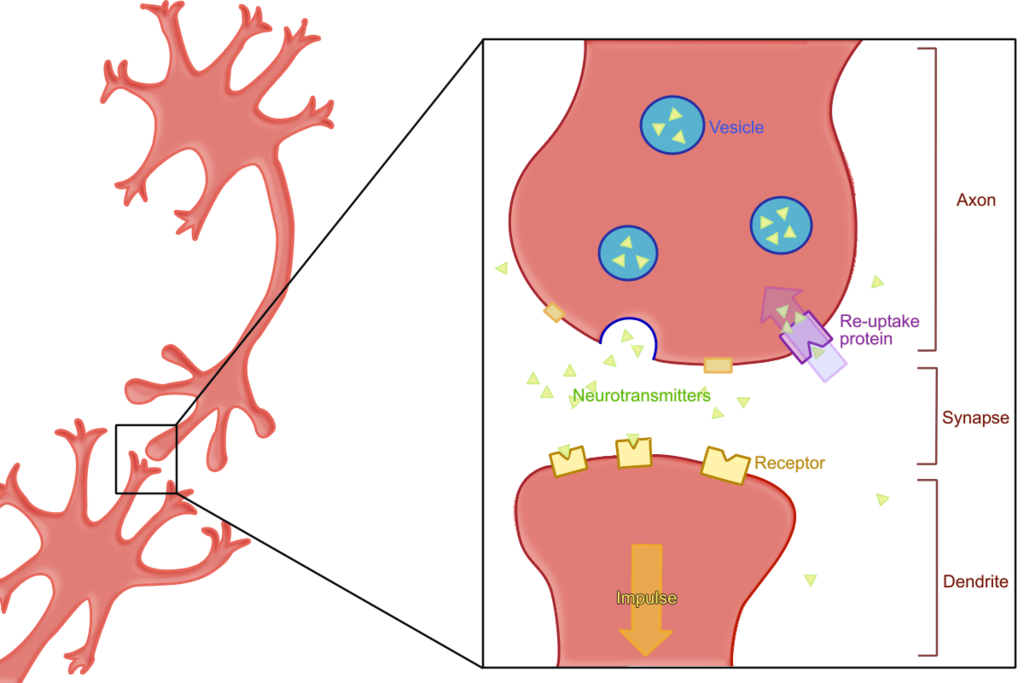
Next, we should consider the synapse - the connection of two neurons. It is important for us because it is in the synapses that the transmission of nerve impulses occurs [6], which, as mentioned above, determines, among other things, whether the subject will be mentally ill or not. At the conceptual level, the synapse looks like this:
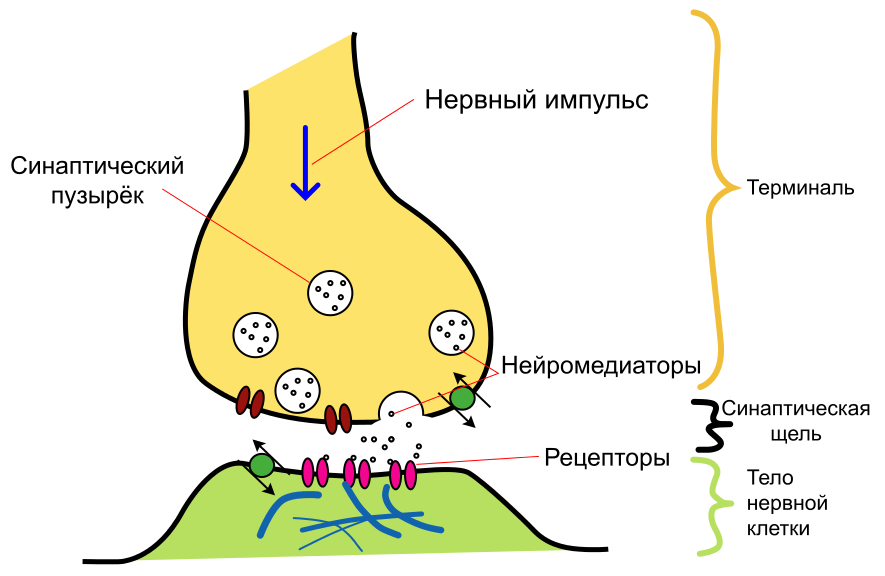
First of all, it should be said that synapses are of two types - chemical and electrical (there are more mixed, but they are not so interesting for us) [7]. In the first, the signal from one neuron to another is transmitted through release into the interneuronal space (the so-called synaptic cleft ) of certain substances ( neurotransmitters or neurotransmitters , depending on which translation you prefer), and secondly, directly, as in the contact of wires , - the current goes from one neuron to another.
We are interested in chemical synapses, since all drugs known and used in psychiatry work with them [4]. In fact, they interfere with the signal transmission process in order to change it in such a way as to reduce the manifestations of the disease. Therefore, we will first have to consider how this signal is transmitted in a natural way, without drugs, then determine what pathological changes in this process take place in the disease, and only then learn how to modify it.
Before proceeding directly to the description of the signal transmission mechanism, we make two important caveats: first, we consider only chemical synapses here, and, second, we present a very simplified description of this process, since the article’s size is limited.
So, everything starts with the impulse that the first neuron sends (it is called presynaptic , because it is located “in front of” the synaptic cleft). An electrical impulse runs along the axon and transmits a signal that a certain number of molecules of the corresponding neurotransmitter should be released into the synaptic cleft from the vesicles (special containers in which the neurotransmitter is stored). [4,6]
Once in the synaptic cleft, the neurotransmitter (primary messenger) binds to the receptors of the postsynaptic (i.e., “second”, located “behind the synaptic cleft”) neuron [4,6].
In addition, in the postsynaptic neuron, the process of further transmission of the message is launched by means of a second messenger — a special intracellular signaling molecule released by the postsynaptic neuron in response to the activation of the postsynaptic receptor (for more information, see below). The secondary messenger orders the postsynaptic neuron to change its ionic fluxes, distribute or inhibit neural electrical impulses, phosphorylate intracellular proteins, and perform many other actions [4].
All this ultimately leads to the fact that in the nucleus of a postsynaptic neuron, expression of certain genes is turned on or off [4,8]. After a change in gene expression, a secondary cascade of events in the postsynaptic neuron is triggered. Many of them are not fully understood [4]. But for the purposes of our article, it suffices to say that this leads (or does not lead) to the generation of a pulse in this neuron and the further transmission of information.
The receptor is a special molecule that is located on the surface of the neuron's membrane and responds by changing the spatial configuration to the accession of a specific substance (neurotransmitter) to it [9]. The substance that activates this receptor is called its ligand .
Chip receptors - in their selectivity. For example, the serotonin receptor does not respond to dopamine and vice versa. This allows you to distinguish between signals from different neurons. Especially given the fact that the neurotransmitter can freely “flow out” of the synaptic cleft and spread throughout the adjacent area [4].
Receptors are (and for us it is important) not only postsynaptic (ie, located on the membrane of the "second" neuron), but presynaptic (ie, located on the membrane of the first neuron). Why are they there? For the organization of feedback: the neuron itself responds to its own neurotransmitter. This is a pretty cool thing, especially since the receptors of one ligand can affect the release of another (below is an example) [4].
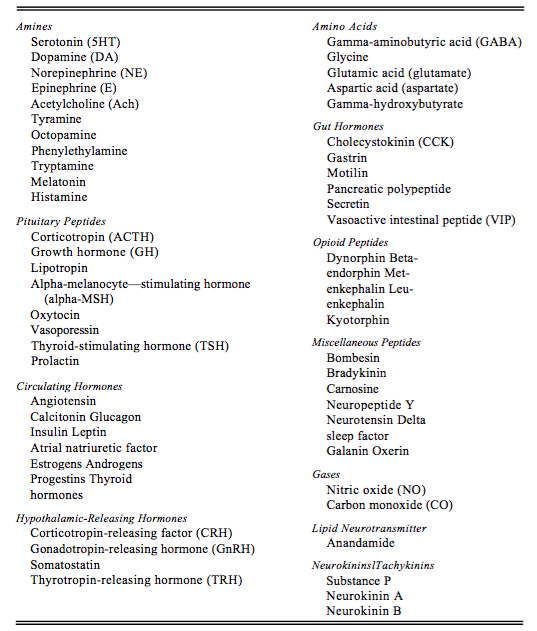
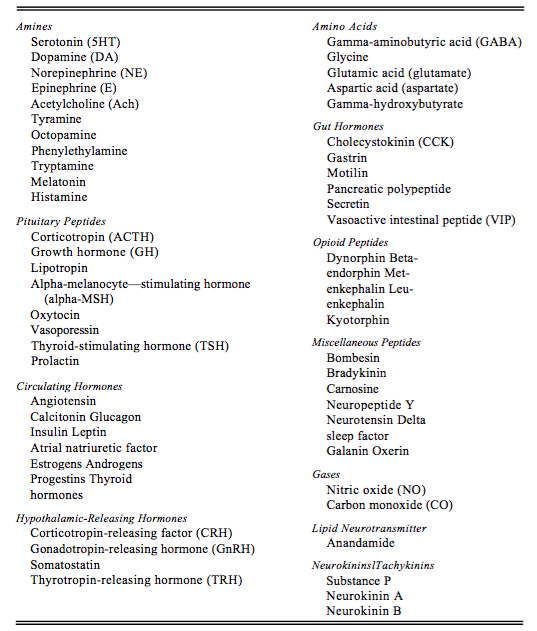
Neurotransmitters (or neurotransmitters ) are the very substances with which a signal is transmitted at a chemical synapse. There are quite a lot of them, the most famous and interesting to us are serotonin, norepinephrine and dopamine.
An example of [incomplete] enumeration of neurotransmitters, divided into groups according to the chemical structure, is presented below [4]:
Psychonauts have a cool saying on this subject: there would be a receptor, and there is a ligand.
We need to remember about neurotransmitters that they are produced by a presynaptic neuron and transmit a message to the postsynaptic one, communicating with its receptors.
According to the principle of action on the receptors, substances can be divided into three (well, four, but those that do not affect the receptor, we are not interested, so three) groups: agonists , antagonists and inverse agonists [4].
Agonists - the easiest thing to understand. They bind to the receptor and cause it to respond. In the text above, when it came to the fact that the neurotransmitter binds to the postsynaptic receptor, he (the neurotransmitter) acted as an agonist.
An antagonist is a ligand that binds to the receptor and “deactivates” it. While the receptor is occupied by an antagonist, an agonist cannot “cling” to it, and, accordingly, the message cannot pass.
An inverse agonist is a substance that, by binding to the receptor, produces physiological effects opposite to those produced by the agonist. Also, it seems, not difficult to understand.
And there are also partial agonists and antagonists - they act in the same way as full, but weaker.
An important consequence: if we use an antagonist of a certain receptor, and then increase the number of neurotransmitter, then in some cases the antagonism will be “canceled”. And back, if we simply reduce the amount of neurotransmitter, the effect will be as if we applied the appropriate antagonist. We will need this consequence later when discussing atypical antipsychotics.
But that is not all. For some neurotransmitters, the so-called mechanism is defined and works. reuptake [10]: hitting the synaptic cleft and passing the message, the neurotransmitter returns back to the vesicle using a special transporter molecule. This is done to save the neurotransmitter and control its quantity in the synaptic cleft.
For each neurotransmitter (more precisely, for each of those that are prone to reuptake) there is its own molecule - the transporter: SERT for serotonin, DAT - for dopamine, etc.
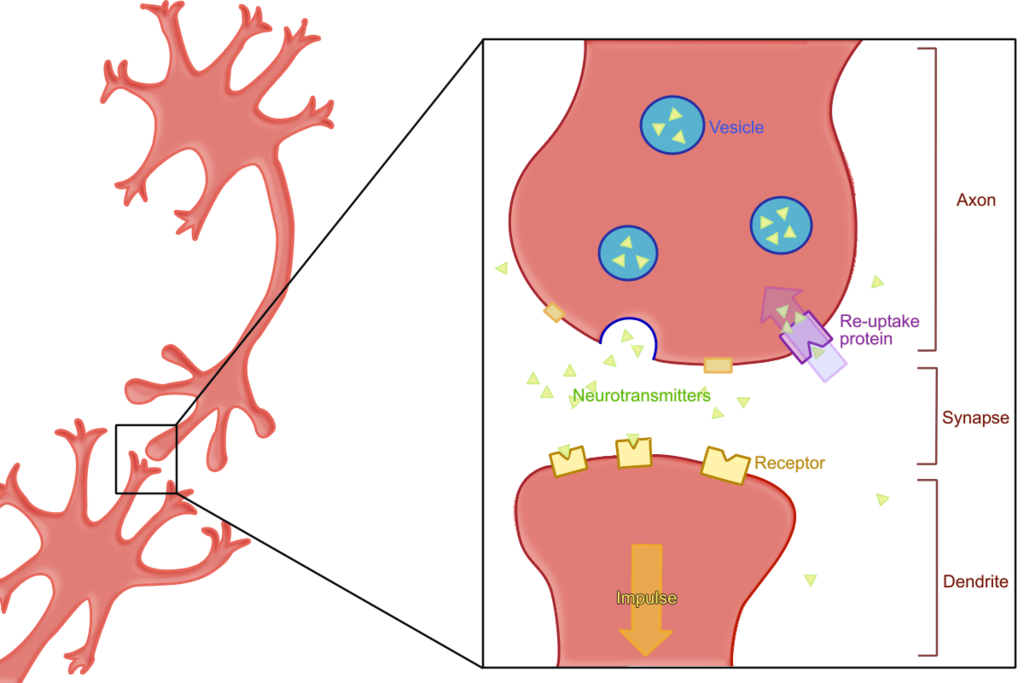
It should be noted the selectivity of the mechanism of reuptake - the transporter can not capture the "alien molecule."
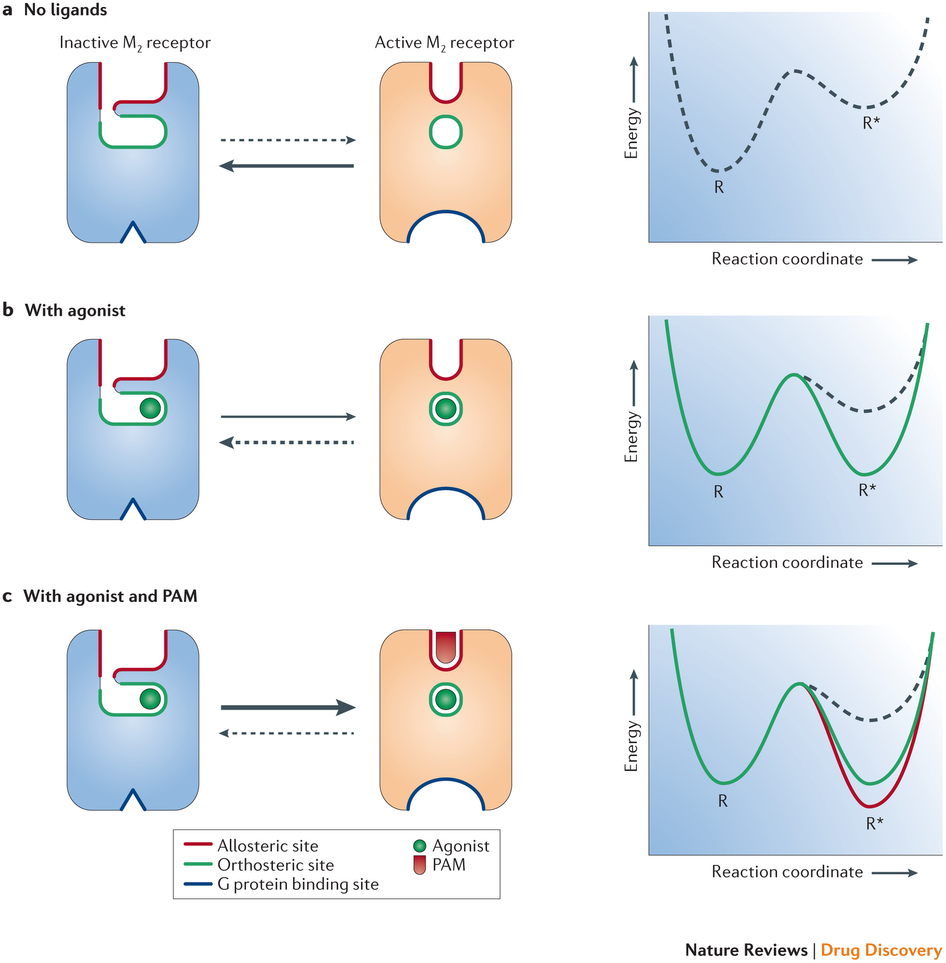
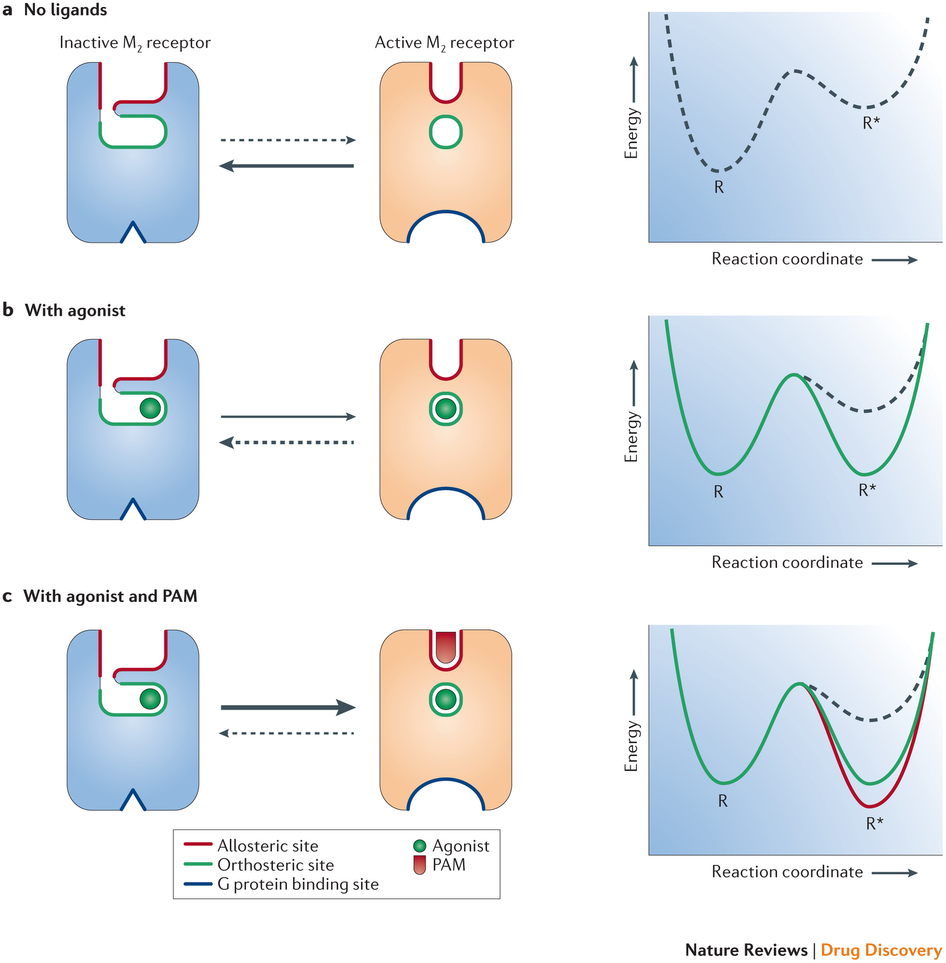
The essence of this phenomenon can be expressed as follows [4]: some receptors are able to interact not only with one ligand, but with two substances. In this case, the first is “basic” and works without the second, and the second affects the receptor only in conjunction with the first, reducing ( allosteric inhibition ) or increasing ( allosteric activation ) response intensity.
- It should be noted that the brain work outlined here is very much simplified, and in fact everything is much more complicated there.
So, we have considered the main stages of the transmission of a nerve impulse from one neuron to another. Now we can discuss the mechanisms of the work of psychopharmacological drugs in general [4].
What can we do with these drugs? A lot of things, in fact. First, the drug can act as a direct agonist (dopaminomimetic) or antagonist (neuroleptics) of the corresponding receptors.
Secondly, it can play the role of an inhibitor (SSRI is a class of antidepressants) or an inverter (amphetamine) of the neurotransmitter reuptake process. In the first case, the neurotransmitter will not be removed from the synaptic cleft, in the second, the reuptake system “turns 180 degrees” and instead of pulling the neurotransmitter into vesicles, it starts to release it from them into the synaptic cleft.
Thirdly, it is possible to influence the system of secondary mediators (according to some data, some of the mood agents do just that) by changing the cascade of events in the receiving (postsynaptic) neuron.
Fourth, it is possible to act on the presynaptic receptor, block it, thereby disabling the negative feedback mechanism and increasing the number of neurotransmitter in the synaptic cleft (some antidepressants and atypical neuroleptics).
Fifth, one can use the mechanism of allosteric modulation and enhance or weaken the effect of the corresponding neurotransmitters.
And finally, sixthly, you can influence the expression of genes. Drugs in which this mechanism would be basic, are unknown to us, but, for example, valproates possess this property [11].
“Mental illness by default” in our mental hospitals (taking this opportunity, we convey hello to LS and other psychiatrists who are used to putting it up without understanding it all in a row), so well-known that it became a curse (remember all these “hell-hurt” and “ You're a stunner. ")
A small enough believable video that allows you to look inside the schizophrenic perception:
In short, it manifests itself in two aspects: negative and productive symptoms [12]. Productive symptoms - this is when the psyche begins to produce something that normally it should not produce: hallucinations, relationship ideas, delusions.
Examples? The author, for example, often sees non-existent cats. One patient, with whom I had to work, felt that he was “fucked for dreams.” Another believed that only the FSB's intrigues prevented him from receiving a reward for hacking the RSA algorithm. A third thought that the cunning Chinese were pouring heroin on marijuana and making him a drug addict. There is a popular case in the literature in which the patient believed that dogs were looking at him and laughing at his frail body [13].
Negative symptoms are the opposite, when the psyche does not produce what it should. This includes volitional decline (the patient cannot bring himself to wash or even eat), emotional flattening (the patient is not able to express emotions, it seems insensitive) and intellectual decline.
Let's make a reservation that here by schizophrenia we mean not only F20, but the whole spectrum of schizophren-like disorders F2X, perhaps, with the exception of schizoaffective (F25), which in some cases is closer to affective disorders (we will discuss them later).
There are quite a few hypotheses regarding the causes of schizophrenia [4,13]: “downed life trajectory” of psychoanalysts, violation of the rules of abstraction and context (Bateson's theory), the invasion of Grofov's transpersonal entities, violation of dopaminergic transmission, etc.
In this article we will consider the latter, since the majority of drugs widely used in psychiatry affect the dopamine system (well, and serotonin, but these are subtleties).
So, in our brain there is such a thing as a black body (Substantia nigra) - an accumulation of dopamine bodies (ie, those that use dopamine as a means of transmitting information) of neurons. From there, axons of these neurons stretch to different areas of the brain, forming so-called. dopaminergic pathways: mesocortical , mesolimbic , nigrostrial and tuberoinfundibular [4].

Consider their connection with the manifestations of schizophrenia. The most interesting for us will be the mesolimbic dopamine pathway connecting the midbrain tire and the substantia nigra with various structures of the limbic system. Indirectly, it is also projected on the frontal cortex and hypothalamus. Normally, it plays an important role in the process of learning, reward, memory and emotion mechanisms [4].
It was found that drugs that increase dopaminergic transmission in this way lead to the appearance of psychotic symptoms (delusions, hallucinations - positive symptoms). On the other hand, drugs that reduce the level of dopamine in these areas have the ability to relieve such symptoms. An interesting fact: the psychosis caused by the systematic abuse of stimulants - cocaine, amphetamine, etc., can be practically indistinguishable from the schizophrenic psychosis by external manifestations [4].
In addition, a link has been established between the excessive activity of impulse transmission in this way and the aggression of patients in psychosis.
The mesocortical way is also very interesting for us, but for a different reason. It connects the ventral region of the midbrain tire with the frontal lobe of the cerebral cortex, mainly the prefrontal cortex, and plays an important role in the processes of motivation, planning and emotional response.
It has been established [4] that a decrease in the level of dopamine in this way is associated with negative symptoms of schizophrenia: a flattening of affect, depletion of emotional life, speech disorders and, probably, a decrease in intelligence.
And what an interesting thing it turns out: in schizophrenia, in one way (mesolimbic) you need to reduce the level of dopamine, and in the other (mesocortical) - increase [4]. It must be said that modern psychopharmacology has partially solved this task, we will explain in what way, for now we briefly consider the remaining two ways in the context of the question that interests us.
The nigrostriatal path connecting the black substance and the ventral region of the midbrain tire with the striatum participates in the initiation of motor activity, being part of a system called the motor loop of the basal ganglia. It is interesting to us because the lack of dopamine in this way causes akathisia (neuside) - a condition in which the patient experiences a compulsive (insurmountable) need for movement: he is literally unable to sit still. [4] Here is a video of the process:
In itself, akatizia is not a symptom of schizophrenia, but it is associated with it - it is a rather frequent side effect of anti-schizophrenic drugs (I think the logic is clear: they are trying to reduce dopamine levels in the mesolimbic pathway with drugs, and it decreases in the nigrostriar way). And there is such a thing as neuroleptic-induced dyskinesia - the pathological movements of arbitrary muscle groups ("twists"). And she is on YouTube:
And finally, the tuberoinfundibular pathway formed by the dopaminergic neynaromas of the arcuate nucleus of the mediobasal hypothalamus projecting their axons into the median elevation. The dopamine secreted by them regulates the secretion of prolactin by the anterior part of the pituitary gland [4]. We are interested in it in so far as many antipsychotic drugs lead to an increase in the level of prolactin, which is especially critical for women: they lose their menstrual cycle and lactation can begin.

Generally speaking, this class of drugs is not only used to treat schizophrenia, but they are associated with it. Historically divided into two large groups - typical and atypical .
Typical neuroleptics include such well-known drugs as haloperidol, chlorpromazine ("Aminazin"), trifluoperazin ("Triftazin"). Strictly speaking, neuroleptics, i.e. drugs that cause neurolepsy - a state of significant reduction in motor and mental activity, emotional flatness and indifference to what is happening, are only drugs of this group. It is more correct to call newer, atypical, “neuroleptics” antipsychotics, but no one really bothers about this.
The main mechanism of action of these drugs is to block postsynaptic dopamine receptors (mainly D2) [4,14]. From the mechanism described above for the onset of schizophrenia, it is clear what the therapeutic effect of these drugs is based on: they block receptors in the mesolimbic path (remember that receptor antagonists make these same receptors inactive, causing the signal to cease to be transmitted from one neuron to another).
The only bad thing is that typical neuroleptics are not limited to affecting the mesolimbic pathway, also blocking the D2 receptors in the mesocortical pathway, which leads to worsening of negative symptoms (think that they manifest precisely because of insufficient dopaminergic transmission in this path) [4 ]. That is, in fact, they work according to the well-known principle: “we treat one, cripple the other”.
And if we consider that the combination of productive and negative symptoms in schizophrenia is not at all uncommon, then everything becomes completely sad (negative symptoms, all other things being equal, mean a less favorable long-term prognosis than productive ones). To reduce the undesirable effects of taking antipsychotics, special preparations are used, correctors , the most famous of which is trihexyphenidyl (Cyclodol).
In general, in our experience, it is difficult to distinguish a person who has strongly pronounced negative symptoms of schizophrenia from a patient who is “dumbfounded” with antipsychotics.
Differences are not visible not only visually or when communicating, but also by tests. It often happens that the replacement of a typical neuroleptic with a more modern drug significantly reduces the severity of intellectual deficit, volitional decline, emotional flattening and other negative symptoms.
But this is not all bad, what can be said about these drugs. Since they block D2 receptors absolutely everywhere, incl. in the nigrostrial way, they are the cause of such phenomena as akathisia (“non-muslin”) and dyskinesia (“twisting”) [4].
And almost all the drugs in this group lead to an increase in the level of prolactin, with all the ensuing consequences (gee-gee, Beavis, pun).
These are the pills. At the same time, they are the most popular drugs of choice in mental hospitals, at least in our region. Why? There are two reasons for this.
The first is quite rational: they perfectly allow you to remove the state of acute psychosis [4]. If the patient is aggressive, in agitation, he sees voices and hears aliens, runs after the household with an ax, etc., then a shot of life-giving haloperidol (or another drug of this group) is able to bring it to a state that is suitable, if not for conversation, then for transportation institution, much faster than more modern drugs. Not always, but this is the trend.
The second reason is the banal lack of funding. It often happens that a psychiatrist would be happy to prescribe some aripiprazole, but it simply does not exist and will never be in the first-aid kit because it is quite expensive.
Well, you need to say separately: if your psychiatrist has assigned you a typical neuroleptic, do not rush to quarter it - sometimes they can really be the best choice. But the consideration of such subtleties is already beyond the scope of this article.
Now let's talk about atypical antipsychotics (they are simply “ atypicals ”). Typical representatives of the atypical antipsychotic group are quetiapine, olanzapine, risperidone, etc.

As mentioned above, the main problem with typical neuroleptics is that they equally block dopaminergic transmission in all four dopamine pathways, while ideally we only need to block it in one, in one - strengthen it, and the other two, If possible, do not touch.
Atypics partially solve this problem [4]. In terms of pharmacology, they are antagonists of dopamine and serotonin receptors. As you can see, serotonin was added here, which was not in the description of schizophrenia itself (the reader with an asterisk knows about the role of 5-HT-2A receptors, but we decided not to complicate the picture).
The fact is that serotonin inhibits the release of dopamine, and the nature of this inhibition differs in all four dopamine pathways. Thus, by affecting serotonin, we can influence dopamine (indirectly). Let's try to figure it out.
Dopamine (i.e., those that transmit information through dopamine) have a postsynaptic serotonin receptor, by activating which, we can reduce the release of dopamine. In fact, it works like a switch: by stimulating the serotonin receptor (5-HT-2A), we inhibit the release of dopamine into the synaptic cleft. The opposite is also true: by blocking the serotonin receptor (5-HT-2A), we increase the release of dopamine. Those. oppose its antagonism.
Here it is important to understand: atypics simultaneously act in opposite directions: they reduce dopaminergic transmission by antagonizing D2-dopamine receptors and increase it by blocking 5-HT-2A-serotonin receptors. What action "win" depends on the number of 5-HT-2ª receptors [4].
Fortunately, they are least of all in the mesolimbic pathway. This means that there the D2 receptor antagonism “wins” and dopaminergic transmission decreases, which is what we need, since this leads to a decrease in productive symptoms.
In the nigrostrial pathway (which is responsible for dyskinesia and akathisia), the additional release of dopamine by blocking 5-HT-2A-serotonin receptors compensates for the effects of atypics as D2 receptor agonists.
In the mesocortical pathway, serotonin receptors are more dense than dopamine receptors, so the atypics work to increase dopaminergic transmission, which is what we need, since this allows us to deal with negative symptoms. Again, nature itself seems to play along with us.
An interesting fact about atipikah is that in fact the victory of one action over another (increasing dopaminergic transmission over its decrease or vice versa) depends not only on which way it is, but also on the dose of the drug. Therefore, they (atypics) have a very strong dependence of the clinical effect on the dose of the drug [4].
Finally, the most interesting are the atypics of the third generation - aripiprazole and bifenprox.

They are interesting in that they simultaneously have the properties of partial agonists and antagonists of dopamine (D2) and serotonin (5-HT-1A) receptors [15]. What particular properties of the drug will manifest depends on the dose and on the presence and amount of the neurotransmitter.
This makes the pharmacological profile of these drugs unique: if there is little dopamine, they work as an activator of dopaminergic transmission, and if its dose is low, then it acts as its inhibitor.
A review of antipsychotics would be incomplete without a description of the personal experience of taking this group of drugs. Next, I will briefly talk about how it was. Please do not take it as a guide to action, since the selection of the psychopharma is an individual process and should be carried out under the guidance of a specialist.
Quetiapine - took for relief of manic episodes. He copes with this task perfectly, but he didn’t like it all the time: emotional flattening is too strong and I really want to sleep. I use it occasionally for the purpose of escaping from reality in case of emotionally significant events that are not in a position to bear as a safety net when receiving% ROSCOMNADZOR%.
Chlorpromazine("Aminazin") - did not like at all. Violations of thinking do not remove at all, very sedatively, shorten associative chains, interfere with thinking. It does nothing, makes it worse.
Amisulpride . The effect is dose dependent. At 400 mg / day. sensations - as if you live in a basin with glycerin: movements are slow, physically you feel air resistance, reality is clouded. It is impossible to think, to express emotions too. At 50 mg - you activate, it seems easy, thinking disorders are significantly less pronounced.
Aripiprazole . Now I am writing on it (in combination with some other drugs) this article, which I could not even dream of before.
- The article turned out to be quite large, and therefore we will tell about the treatment of affective disorders (depression, mania), OCD, GAD and other things in the next article if this topic will be interesting to the community at all.
1. Douglas Fields. Glial cells (neuroglia).
scisne.net/a-1101
2. Konorev, M.R. A course of lectures on pharmacology: a manual for students of the 3rd and 4th courses pharmacist. a fact honey.of universities: in 2 volumes. T. 1: / M. R. Konorev, I. I. Krapivko, D. A. Rozhdestvensky; Ministry of Health of the Republic of Belarus, Vitebsk State. honey.un-t - Vitebsk: [VSMU], 2013. - 243 p
. E 3. F. Huho. Neurochemistry. Basics and principles. M .: Mir, 1990. ISBN 5-003-001030-0
4. Stahl, SM Essential psychopharmacology: neuroscientific basis and practical application / Stephen M. Stahl; with illustrations by Nancy Muntner. — 2nd ed. p .; cm. ISBN 0-521-64154-3 (hardback) —ISBN 0-521-64615-4 (pbk.)
5. Neurochemistry: a textbook for biological and medical universities. Ed. Acad.RAMS I.P. Ashmarin and prof. P.V.Stukalov. M .: Izd. Institute of Biomedical Chemistry, RAMS, 1996. ISBN: 5-900760-02-2
6. Shostak V.I., Lytaev S.A., Berezantseva M.S. Psychophysiology. Tutorial. - SPb, 2007. ISBN 978-5-93979-186-1
7. Eccles DK The physiology of synapses. - M .: Mir, 1966. - 397 p.
8. Anne E. West, Wen G. Chen, Matthew B. Dalva, Ricardo E. Dolmetsch, Jon M. Kornhauser, Adam J. Shaywitz, Mari A. Takasu, Xu Tao, and Michael E. Greenberg. Calcium regulation of neuronal gene expression PNAS 2001 98 (20) 11024-11031; doi: 10.1073 / pnas.191352298
9. John E. Hall PhD. Guyton and Hall Textbook of Medical Physiology, 13e (Guyton Physiology). ISBN-13: 978-1455770052
10. Neurotransmitter Transporters in the Central Nervous System J. Masson, C. Sagné, M. Hamon and S. El Mestikawy. Pharmacological Reviews September 1, 1999, 51 (3) 439-464;
11. Guang Chen, Pei-Xong Yuan, Yi-Ming Jiang, Li-Dong Huang, Husseini K. Manji. Valproate robustly enhances AP-1 mediated gene expression. Molecular Brain Research. 22 January 1999
12. Bukhanovsky A.O. et al. General psychopathology: a manual for doctors. / A.O. Bukhanovsky, Yu.A. Kutyavin, M.E. Litvak. - 3rd ed., Outgrown. and add.- Rostov n / D: Publishing house of LRNTs "Phoenix", 2003
13. Michael Garrett. CBT for psychosis in a psychoanalytic frame. Seminar.
14. Farde L, Nordström A, Wiesel F, Pauli S, Halldin C, Sedvall G. Positron Dopamine Receptor for Patient Drops and Dopamine Receptor. Arch Gen Psychiatry. 1992; 49 (7): 538-544. doi: 10.1001 / archpsyc.1992.01820070032005
15. Abilify (Aripiprazole) - Description and Clinical Pharmacology.
www.druglib.com/druginfo/abilify/description_pharmacology
This article is a logical continuation of the post devoted to pathopsychological diagnosis. In it, I will try to speak in an accessible language about the main groups of pharmacological drugs used to treat mental diseases, as well as about the mechanisms, structures and components of the human brain that are involved in this process.
')
Disclaimer : I am not a psychiatrist, but a psycho. I tested the drugs of all these groups on myself and watched their actions (when I was in an insane asylum). In addition, I have some experience in selecting pharmacy, but I do not have a formal education in this area. In this regard, as well as the fact that making a diagnosis according to scientific articles is an extremely wrong thing in its basis, I want to warn the reader that, before accepting any of the things described here, you must consult with a specialist. If real welders come to the post and substantiate the incorrectness of the stated theses, I will be only glad.
If the above does not scare you, I suggest to plunge into the fascinating world of psychopharmacology. In the post a lot of letters and pictures, I warn you immediately.
Brain and its structure in the context of psychopharmacology
Before talking about the pharmacological methods of treating mental illness, it is necessary to consider some aspects of the structure and functioning of the human brain - just so that further material is clear.
Neurons and glia
Most likely, everyone present knows that the brain consists of neurons and neuroglia (special cells that perform a variety of functions - trophic, structural, secretory, regulatory and protective [1, 3]) - the first are the main objects of our interest, the second is not so important for this article, since most modern pharmacology has no significant effect on it (more precisely, it has only in the context of side effects).
Neurons look like this:
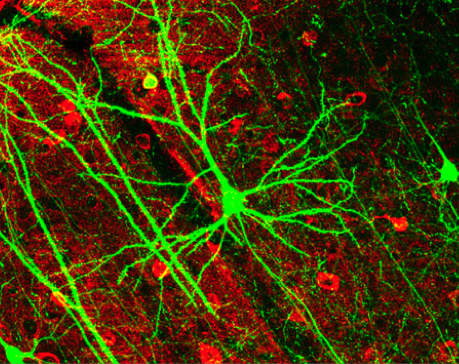
And glial cells - like this:
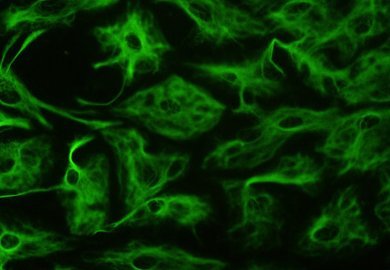
Contrary to popular belief, glial cells are quite involved in the transmission of nerve impulses [1], at least indirectly - by influencing the formation of synapses (about them - below), but all the drugs we know do not affect its cells and functions, but neurons and communication between them [4].
Consider an approximate model of the structure of the neuron:
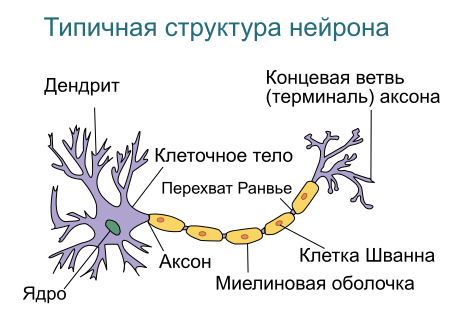
We are interested in dendrites - processes, through which a neuron receives messages from its fellows [6] (roughly speaking, the input of a neuron) and an axon - a process through which a neuron transmits its message (ie its “output”) [6].
Why is that? Because they are directly related to the signals that the neurons transmit to each other, and in these signals the whole “spiritual life” of a person (well, almost all) is encrypted: his thoughts, memories, beliefs, preferences, etc., including Of course, what is considered a manifestation of mental illness is delusional concepts, hallucinations, and so on [4].
Thus, the task of treating mental diseases is reduced (within the framework of the biologizing approach , namely, it is the basis of this article, we will talk about others separately) to the task of changing the parameters of the passage of signals between neurons and those events that occur in the neurons themselves due to this transfer [4]. Of course, not an arbitrary change, but a directed and controlled one.
Synapses
Next, we should consider the synapse - the connection of two neurons. It is important for us because it is in the synapses that the transmission of nerve impulses occurs [6], which, as mentioned above, determines, among other things, whether the subject will be mentally ill or not. At the conceptual level, the synapse looks like this:
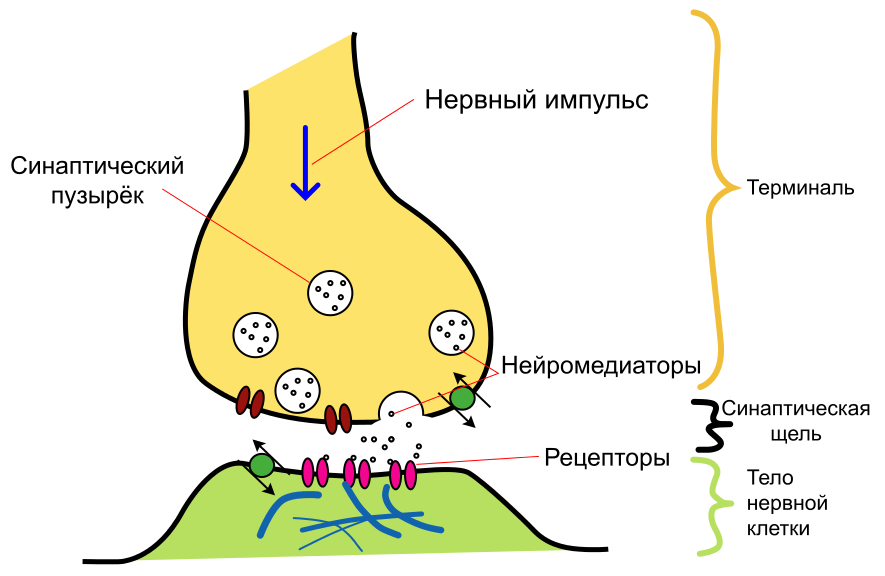
First of all, it should be said that synapses are of two types - chemical and electrical (there are more mixed, but they are not so interesting for us) [7]. In the first, the signal from one neuron to another is transmitted through release into the interneuronal space (the so-called synaptic cleft ) of certain substances ( neurotransmitters or neurotransmitters , depending on which translation you prefer), and secondly, directly, as in the contact of wires , - the current goes from one neuron to another.
We are interested in chemical synapses, since all drugs known and used in psychiatry work with them [4]. In fact, they interfere with the signal transmission process in order to change it in such a way as to reduce the manifestations of the disease. Therefore, we will first have to consider how this signal is transmitted in a natural way, without drugs, then determine what pathological changes in this process take place in the disease, and only then learn how to modify it.
Signal transmission between neurons
Before proceeding directly to the description of the signal transmission mechanism, we make two important caveats: first, we consider only chemical synapses here, and, second, we present a very simplified description of this process, since the article’s size is limited.
So, everything starts with the impulse that the first neuron sends (it is called presynaptic , because it is located “in front of” the synaptic cleft). An electrical impulse runs along the axon and transmits a signal that a certain number of molecules of the corresponding neurotransmitter should be released into the synaptic cleft from the vesicles (special containers in which the neurotransmitter is stored). [4,6]
Once in the synaptic cleft, the neurotransmitter (primary messenger) binds to the receptors of the postsynaptic (i.e., “second”, located “behind the synaptic cleft”) neuron [4,6].
In addition, in the postsynaptic neuron, the process of further transmission of the message is launched by means of a second messenger — a special intracellular signaling molecule released by the postsynaptic neuron in response to the activation of the postsynaptic receptor (for more information, see below). The secondary messenger orders the postsynaptic neuron to change its ionic fluxes, distribute or inhibit neural electrical impulses, phosphorylate intracellular proteins, and perform many other actions [4].
All this ultimately leads to the fact that in the nucleus of a postsynaptic neuron, expression of certain genes is turned on or off [4,8]. After a change in gene expression, a secondary cascade of events in the postsynaptic neuron is triggered. Many of them are not fully understood [4]. But for the purposes of our article, it suffices to say that this leads (or does not lead) to the generation of a pulse in this neuron and the further transmission of information.
The receptors
The receptor is a special molecule that is located on the surface of the neuron's membrane and responds by changing the spatial configuration to the accession of a specific substance (neurotransmitter) to it [9]. The substance that activates this receptor is called its ligand .
Chip receptors - in their selectivity. For example, the serotonin receptor does not respond to dopamine and vice versa. This allows you to distinguish between signals from different neurons. Especially given the fact that the neurotransmitter can freely “flow out” of the synaptic cleft and spread throughout the adjacent area [4].
Receptors are (and for us it is important) not only postsynaptic (ie, located on the membrane of the "second" neuron), but presynaptic (ie, located on the membrane of the first neuron). Why are they there? For the organization of feedback: the neuron itself responds to its own neurotransmitter. This is a pretty cool thing, especially since the receptors of one ligand can affect the release of another (below is an example) [4].
Neurotransmitters
Neurotransmitters (or neurotransmitters ) are the very substances with which a signal is transmitted at a chemical synapse. There are quite a lot of them, the most famous and interesting to us are serotonin, norepinephrine and dopamine.
An example of [incomplete] enumeration of neurotransmitters, divided into groups according to the chemical structure, is presented below [4]:
Psychonauts have a cool saying on this subject: there would be a receptor, and there is a ligand.
We need to remember about neurotransmitters that they are produced by a presynaptic neuron and transmit a message to the postsynaptic one, communicating with its receptors.
Agonists, antagonists and inverse agonists
According to the principle of action on the receptors, substances can be divided into three (well, four, but those that do not affect the receptor, we are not interested, so three) groups: agonists , antagonists and inverse agonists [4].
Agonists - the easiest thing to understand. They bind to the receptor and cause it to respond. In the text above, when it came to the fact that the neurotransmitter binds to the postsynaptic receptor, he (the neurotransmitter) acted as an agonist.
An antagonist is a ligand that binds to the receptor and “deactivates” it. While the receptor is occupied by an antagonist, an agonist cannot “cling” to it, and, accordingly, the message cannot pass.
An inverse agonist is a substance that, by binding to the receptor, produces physiological effects opposite to those produced by the agonist. Also, it seems, not difficult to understand.
And there are also partial agonists and antagonists - they act in the same way as full, but weaker.
An important consequence: if we use an antagonist of a certain receptor, and then increase the number of neurotransmitter, then in some cases the antagonism will be “canceled”. And back, if we simply reduce the amount of neurotransmitter, the effect will be as if we applied the appropriate antagonist. We will need this consequence later when discussing atypical antipsychotics.
Reverse capture of neurotransmitters
But that is not all. For some neurotransmitters, the so-called mechanism is defined and works. reuptake [10]: hitting the synaptic cleft and passing the message, the neurotransmitter returns back to the vesicle using a special transporter molecule. This is done to save the neurotransmitter and control its quantity in the synaptic cleft.
For each neurotransmitter (more precisely, for each of those that are prone to reuptake) there is its own molecule - the transporter: SERT for serotonin, DAT - for dopamine, etc.
It should be noted the selectivity of the mechanism of reuptake - the transporter can not capture the "alien molecule."
Allosteric modulation
The essence of this phenomenon can be expressed as follows [4]: some receptors are able to interact not only with one ligand, but with two substances. In this case, the first is “basic” and works without the second, and the second affects the receptor only in conjunction with the first, reducing ( allosteric inhibition ) or increasing ( allosteric activation ) response intensity.
- It should be noted that the brain work outlined here is very much simplified, and in fact everything is much more complicated there.
Mental diseases and their treatment
Principles of work of psychopharma
So, we have considered the main stages of the transmission of a nerve impulse from one neuron to another. Now we can discuss the mechanisms of the work of psychopharmacological drugs in general [4].
What can we do with these drugs? A lot of things, in fact. First, the drug can act as a direct agonist (dopaminomimetic) or antagonist (neuroleptics) of the corresponding receptors.
Secondly, it can play the role of an inhibitor (SSRI is a class of antidepressants) or an inverter (amphetamine) of the neurotransmitter reuptake process. In the first case, the neurotransmitter will not be removed from the synaptic cleft, in the second, the reuptake system “turns 180 degrees” and instead of pulling the neurotransmitter into vesicles, it starts to release it from them into the synaptic cleft.
Thirdly, it is possible to influence the system of secondary mediators (according to some data, some of the mood agents do just that) by changing the cascade of events in the receiving (postsynaptic) neuron.
Fourth, it is possible to act on the presynaptic receptor, block it, thereby disabling the negative feedback mechanism and increasing the number of neurotransmitter in the synaptic cleft (some antidepressants and atypical neuroleptics).
Fifth, one can use the mechanism of allosteric modulation and enhance or weaken the effect of the corresponding neurotransmitters.
And finally, sixthly, you can influence the expression of genes. Drugs in which this mechanism would be basic, are unknown to us, but, for example, valproates possess this property [11].
Schizophrenia
“Mental illness by default” in our mental hospitals (taking this opportunity, we convey hello to LS and other psychiatrists who are used to putting it up without understanding it all in a row), so well-known that it became a curse (remember all these “hell-hurt” and “ You're a stunner. ")
A small enough believable video that allows you to look inside the schizophrenic perception:
In short, it manifests itself in two aspects: negative and productive symptoms [12]. Productive symptoms - this is when the psyche begins to produce something that normally it should not produce: hallucinations, relationship ideas, delusions.
Examples? The author, for example, often sees non-existent cats. One patient, with whom I had to work, felt that he was “fucked for dreams.” Another believed that only the FSB's intrigues prevented him from receiving a reward for hacking the RSA algorithm. A third thought that the cunning Chinese were pouring heroin on marijuana and making him a drug addict. There is a popular case in the literature in which the patient believed that dogs were looking at him and laughing at his frail body [13].
Negative symptoms are the opposite, when the psyche does not produce what it should. This includes volitional decline (the patient cannot bring himself to wash or even eat), emotional flattening (the patient is not able to express emotions, it seems insensitive) and intellectual decline.
Let's make a reservation that here by schizophrenia we mean not only F20, but the whole spectrum of schizophren-like disorders F2X, perhaps, with the exception of schizoaffective (F25), which in some cases is closer to affective disorders (we will discuss them later).
There are quite a few hypotheses regarding the causes of schizophrenia [4,13]: “downed life trajectory” of psychoanalysts, violation of the rules of abstraction and context (Bateson's theory), the invasion of Grofov's transpersonal entities, violation of dopaminergic transmission, etc.
In this article we will consider the latter, since the majority of drugs widely used in psychiatry affect the dopamine system (well, and serotonin, but these are subtleties).
So, in our brain there is such a thing as a black body (Substantia nigra) - an accumulation of dopamine bodies (ie, those that use dopamine as a means of transmitting information) of neurons. From there, axons of these neurons stretch to different areas of the brain, forming so-called. dopaminergic pathways: mesocortical , mesolimbic , nigrostrial and tuberoinfundibular [4].

Consider their connection with the manifestations of schizophrenia. The most interesting for us will be the mesolimbic dopamine pathway connecting the midbrain tire and the substantia nigra with various structures of the limbic system. Indirectly, it is also projected on the frontal cortex and hypothalamus. Normally, it plays an important role in the process of learning, reward, memory and emotion mechanisms [4].
It was found that drugs that increase dopaminergic transmission in this way lead to the appearance of psychotic symptoms (delusions, hallucinations - positive symptoms). On the other hand, drugs that reduce the level of dopamine in these areas have the ability to relieve such symptoms. An interesting fact: the psychosis caused by the systematic abuse of stimulants - cocaine, amphetamine, etc., can be practically indistinguishable from the schizophrenic psychosis by external manifestations [4].
In addition, a link has been established between the excessive activity of impulse transmission in this way and the aggression of patients in psychosis.
The mesocortical way is also very interesting for us, but for a different reason. It connects the ventral region of the midbrain tire with the frontal lobe of the cerebral cortex, mainly the prefrontal cortex, and plays an important role in the processes of motivation, planning and emotional response.
It has been established [4] that a decrease in the level of dopamine in this way is associated with negative symptoms of schizophrenia: a flattening of affect, depletion of emotional life, speech disorders and, probably, a decrease in intelligence.
And what an interesting thing it turns out: in schizophrenia, in one way (mesolimbic) you need to reduce the level of dopamine, and in the other (mesocortical) - increase [4]. It must be said that modern psychopharmacology has partially solved this task, we will explain in what way, for now we briefly consider the remaining two ways in the context of the question that interests us.
The nigrostriatal path connecting the black substance and the ventral region of the midbrain tire with the striatum participates in the initiation of motor activity, being part of a system called the motor loop of the basal ganglia. It is interesting to us because the lack of dopamine in this way causes akathisia (neuside) - a condition in which the patient experiences a compulsive (insurmountable) need for movement: he is literally unable to sit still. [4] Here is a video of the process:
In itself, akatizia is not a symptom of schizophrenia, but it is associated with it - it is a rather frequent side effect of anti-schizophrenic drugs (I think the logic is clear: they are trying to reduce dopamine levels in the mesolimbic pathway with drugs, and it decreases in the nigrostriar way). And there is such a thing as neuroleptic-induced dyskinesia - the pathological movements of arbitrary muscle groups ("twists"). And she is on YouTube:
And finally, the tuberoinfundibular pathway formed by the dopaminergic neynaromas of the arcuate nucleus of the mediobasal hypothalamus projecting their axons into the median elevation. The dopamine secreted by them regulates the secretion of prolactin by the anterior part of the pituitary gland [4]. We are interested in it in so far as many antipsychotic drugs lead to an increase in the level of prolactin, which is especially critical for women: they lose their menstrual cycle and lactation can begin.
Antipsychotics (aka antipsychotics)

Generally speaking, this class of drugs is not only used to treat schizophrenia, but they are associated with it. Historically divided into two large groups - typical and atypical .
Typical neuroleptics include such well-known drugs as haloperidol, chlorpromazine ("Aminazin"), trifluoperazin ("Triftazin"). Strictly speaking, neuroleptics, i.e. drugs that cause neurolepsy - a state of significant reduction in motor and mental activity, emotional flatness and indifference to what is happening, are only drugs of this group. It is more correct to call newer, atypical, “neuroleptics” antipsychotics, but no one really bothers about this.
The main mechanism of action of these drugs is to block postsynaptic dopamine receptors (mainly D2) [4,14]. From the mechanism described above for the onset of schizophrenia, it is clear what the therapeutic effect of these drugs is based on: they block receptors in the mesolimbic path (remember that receptor antagonists make these same receptors inactive, causing the signal to cease to be transmitted from one neuron to another).
The only bad thing is that typical neuroleptics are not limited to affecting the mesolimbic pathway, also blocking the D2 receptors in the mesocortical pathway, which leads to worsening of negative symptoms (think that they manifest precisely because of insufficient dopaminergic transmission in this path) [4 ]. That is, in fact, they work according to the well-known principle: “we treat one, cripple the other”.
And if we consider that the combination of productive and negative symptoms in schizophrenia is not at all uncommon, then everything becomes completely sad (negative symptoms, all other things being equal, mean a less favorable long-term prognosis than productive ones). To reduce the undesirable effects of taking antipsychotics, special preparations are used, correctors , the most famous of which is trihexyphenidyl (Cyclodol).
In general, in our experience, it is difficult to distinguish a person who has strongly pronounced negative symptoms of schizophrenia from a patient who is “dumbfounded” with antipsychotics.
Differences are not visible not only visually or when communicating, but also by tests. It often happens that the replacement of a typical neuroleptic with a more modern drug significantly reduces the severity of intellectual deficit, volitional decline, emotional flattening and other negative symptoms.
But this is not all bad, what can be said about these drugs. Since they block D2 receptors absolutely everywhere, incl. in the nigrostrial way, they are the cause of such phenomena as akathisia (“non-muslin”) and dyskinesia (“twisting”) [4].
And almost all the drugs in this group lead to an increase in the level of prolactin, with all the ensuing consequences (gee-gee, Beavis, pun).
These are the pills. At the same time, they are the most popular drugs of choice in mental hospitals, at least in our region. Why? There are two reasons for this.
The first is quite rational: they perfectly allow you to remove the state of acute psychosis [4]. If the patient is aggressive, in agitation, he sees voices and hears aliens, runs after the household with an ax, etc., then a shot of life-giving haloperidol (or another drug of this group) is able to bring it to a state that is suitable, if not for conversation, then for transportation institution, much faster than more modern drugs. Not always, but this is the trend.
The second reason is the banal lack of funding. It often happens that a psychiatrist would be happy to prescribe some aripiprazole, but it simply does not exist and will never be in the first-aid kit because it is quite expensive.
Well, you need to say separately: if your psychiatrist has assigned you a typical neuroleptic, do not rush to quarter it - sometimes they can really be the best choice. But the consideration of such subtleties is already beyond the scope of this article.
Now let's talk about atypical antipsychotics (they are simply “ atypicals ”). Typical representatives of the atypical antipsychotic group are quetiapine, olanzapine, risperidone, etc.

As mentioned above, the main problem with typical neuroleptics is that they equally block dopaminergic transmission in all four dopamine pathways, while ideally we only need to block it in one, in one - strengthen it, and the other two, If possible, do not touch.
Atypics partially solve this problem [4]. In terms of pharmacology, they are antagonists of dopamine and serotonin receptors. As you can see, serotonin was added here, which was not in the description of schizophrenia itself (the reader with an asterisk knows about the role of 5-HT-2A receptors, but we decided not to complicate the picture).
The fact is that serotonin inhibits the release of dopamine, and the nature of this inhibition differs in all four dopamine pathways. Thus, by affecting serotonin, we can influence dopamine (indirectly). Let's try to figure it out.
Dopamine (i.e., those that transmit information through dopamine) have a postsynaptic serotonin receptor, by activating which, we can reduce the release of dopamine. In fact, it works like a switch: by stimulating the serotonin receptor (5-HT-2A), we inhibit the release of dopamine into the synaptic cleft. The opposite is also true: by blocking the serotonin receptor (5-HT-2A), we increase the release of dopamine. Those. oppose its antagonism.
Here it is important to understand: atypics simultaneously act in opposite directions: they reduce dopaminergic transmission by antagonizing D2-dopamine receptors and increase it by blocking 5-HT-2A-serotonin receptors. What action "win" depends on the number of 5-HT-2ª receptors [4].
Fortunately, they are least of all in the mesolimbic pathway. This means that there the D2 receptor antagonism “wins” and dopaminergic transmission decreases, which is what we need, since this leads to a decrease in productive symptoms.
In the nigrostrial pathway (which is responsible for dyskinesia and akathisia), the additional release of dopamine by blocking 5-HT-2A-serotonin receptors compensates for the effects of atypics as D2 receptor agonists.
In the mesocortical pathway, serotonin receptors are more dense than dopamine receptors, so the atypics work to increase dopaminergic transmission, which is what we need, since this allows us to deal with negative symptoms. Again, nature itself seems to play along with us.
An interesting fact about atipikah is that in fact the victory of one action over another (increasing dopaminergic transmission over its decrease or vice versa) depends not only on which way it is, but also on the dose of the drug. Therefore, they (atypics) have a very strong dependence of the clinical effect on the dose of the drug [4].
Finally, the most interesting are the atypics of the third generation - aripiprazole and bifenprox.

They are interesting in that they simultaneously have the properties of partial agonists and antagonists of dopamine (D2) and serotonin (5-HT-1A) receptors [15]. What particular properties of the drug will manifest depends on the dose and on the presence and amount of the neurotransmitter.
This makes the pharmacological profile of these drugs unique: if there is little dopamine, they work as an activator of dopaminergic transmission, and if its dose is low, then it acts as its inhibitor.
Personal experience. Instead of conclusion
A review of antipsychotics would be incomplete without a description of the personal experience of taking this group of drugs. Next, I will briefly talk about how it was. Please do not take it as a guide to action, since the selection of the psychopharma is an individual process and should be carried out under the guidance of a specialist.
Quetiapine - took for relief of manic episodes. He copes with this task perfectly, but he didn’t like it all the time: emotional flattening is too strong and I really want to sleep. I use it occasionally for the purpose of escaping from reality in case of emotionally significant events that are not in a position to bear as a safety net when receiving% ROSCOMNADZOR%.
Chlorpromazine("Aminazin") - did not like at all. Violations of thinking do not remove at all, very sedatively, shorten associative chains, interfere with thinking. It does nothing, makes it worse.
Amisulpride . The effect is dose dependent. At 400 mg / day. sensations - as if you live in a basin with glycerin: movements are slow, physically you feel air resistance, reality is clouded. It is impossible to think, to express emotions too. At 50 mg - you activate, it seems easy, thinking disorders are significantly less pronounced.
Aripiprazole . Now I am writing on it (in combination with some other drugs) this article, which I could not even dream of before.
- The article turned out to be quite large, and therefore we will tell about the treatment of affective disorders (depression, mania), OCD, GAD and other things in the next article if this topic will be interesting to the community at all.
Literature
1. Douglas Fields. Glial cells (neuroglia).
scisne.net/a-1101
2. Konorev, M.R. A course of lectures on pharmacology: a manual for students of the 3rd and 4th courses pharmacist. a fact honey.of universities: in 2 volumes. T. 1: / M. R. Konorev, I. I. Krapivko, D. A. Rozhdestvensky; Ministry of Health of the Republic of Belarus, Vitebsk State. honey.un-t - Vitebsk: [VSMU], 2013. - 243 p
. E 3. F. Huho. Neurochemistry. Basics and principles. M .: Mir, 1990. ISBN 5-003-001030-0
4. Stahl, SM Essential psychopharmacology: neuroscientific basis and practical application / Stephen M. Stahl; with illustrations by Nancy Muntner. — 2nd ed. p .; cm. ISBN 0-521-64154-3 (hardback) —ISBN 0-521-64615-4 (pbk.)
5. Neurochemistry: a textbook for biological and medical universities. Ed. Acad.RAMS I.P. Ashmarin and prof. P.V.Stukalov. M .: Izd. Institute of Biomedical Chemistry, RAMS, 1996. ISBN: 5-900760-02-2
6. Shostak V.I., Lytaev S.A., Berezantseva M.S. Psychophysiology. Tutorial. - SPb, 2007. ISBN 978-5-93979-186-1
7. Eccles DK The physiology of synapses. - M .: Mir, 1966. - 397 p.
8. Anne E. West, Wen G. Chen, Matthew B. Dalva, Ricardo E. Dolmetsch, Jon M. Kornhauser, Adam J. Shaywitz, Mari A. Takasu, Xu Tao, and Michael E. Greenberg. Calcium regulation of neuronal gene expression PNAS 2001 98 (20) 11024-11031; doi: 10.1073 / pnas.191352298
9. John E. Hall PhD. Guyton and Hall Textbook of Medical Physiology, 13e (Guyton Physiology). ISBN-13: 978-1455770052
10. Neurotransmitter Transporters in the Central Nervous System J. Masson, C. Sagné, M. Hamon and S. El Mestikawy. Pharmacological Reviews September 1, 1999, 51 (3) 439-464;
11. Guang Chen, Pei-Xong Yuan, Yi-Ming Jiang, Li-Dong Huang, Husseini K. Manji. Valproate robustly enhances AP-1 mediated gene expression. Molecular Brain Research. 22 January 1999
12. Bukhanovsky A.O. et al. General psychopathology: a manual for doctors. / A.O. Bukhanovsky, Yu.A. Kutyavin, M.E. Litvak. - 3rd ed., Outgrown. and add.- Rostov n / D: Publishing house of LRNTs "Phoenix", 2003
13. Michael Garrett. CBT for psychosis in a psychoanalytic frame. Seminar.
14. Farde L, Nordström A, Wiesel F, Pauli S, Halldin C, Sedvall G. Positron Dopamine Receptor for Patient Drops and Dopamine Receptor. Arch Gen Psychiatry. 1992; 49 (7): 538-544. doi: 10.1001 / archpsyc.1992.01820070032005
15. Abilify (Aripiprazole) - Description and Clinical Pharmacology.
www.druglib.com/druginfo/abilify/description_pharmacology
Source: https://habr.com/ru/post/403189/
All Articles