The history of implantable technology. Pacemaker

The science fiction literature has been telling us about the people of the future - cyborg people for over half a century. We can say that the future has already come - in 2016, cyborg go among us and live a measured life. They are ordinary people, but with pacemakers, auditory implants, prosthetic limbs and biosensors. Today we will talk about the history of the creation of pacemakers, from the bulky Leadville apparatus to modern miniature implants.
The invention of the first pacemaker - Mark Leadville
')
For the first time, anesthesiologist Mark Lidwill applied cardiac pacing. At the meeting of the Australian-Asian Congress in 1929 in Australia, he described the electrical apparatus that drives the human heart. This device applied electrical discharges of varying power and frequency; the monopolar electrode was injected directly into the heart, and the other, indifferent, was applied directly to the skin after wetting in saline solution.
 The doctor told everyone that using a more primitive model of this equipment in 1925 and 1926, he tried to revive the stillborn babies. One of them really came to life and was completely healthy. He noted that this child did not respond to other types of treatment, such as an injection of adrenaline, which was in use in those days. Then Leadville inserted the needle of the electrode first into the right atrium, and then, when the atrial stimulation failed, into the right ventricle. The 10-minute pacemaker had its effect, and when Leadville turned off the pacemaker, the heart started working by itself.
The doctor told everyone that using a more primitive model of this equipment in 1925 and 1926, he tried to revive the stillborn babies. One of them really came to life and was completely healthy. He noted that this child did not respond to other types of treatment, such as an injection of adrenaline, which was in use in those days. Then Leadville inserted the needle of the electrode first into the right atrium, and then, when the atrial stimulation failed, into the right ventricle. The 10-minute pacemaker had its effect, and when Leadville turned off the pacemaker, the heart started working by itself.This patient of Dr. Leadville is considered to be the first person who successfully survived pacemaker, and the Leadville device is considered the first artificial pacemaker. According to the plan of the doctor, the machine was intended for emergency cases, when the patient had a heart stopped under operation under general anesthesia.
Later, the creator of the world's first pacemaker admitted that the device works with varying success, but one saved life of fifty or a hundred is great progress when there is no hope of saving everyone. However, the work of Leadville was then ignored and did not lead to a breakthrough in cardiology.
1930s: Albert Hyman's Artificial Pacemaker
 During intracardiac therapy for cardiac arrest, Albert Hyman from the New York Hospital Beth David noted that the success of this procedure does not depend on the medication used, but is caused by the injection of the needle into the heart. He concluded that when cardiac arrest his electrodynamic balance could be disturbed by one injection, which could lead to myocardial infarction. A few shots could improve the situation, but this is too dangerous.
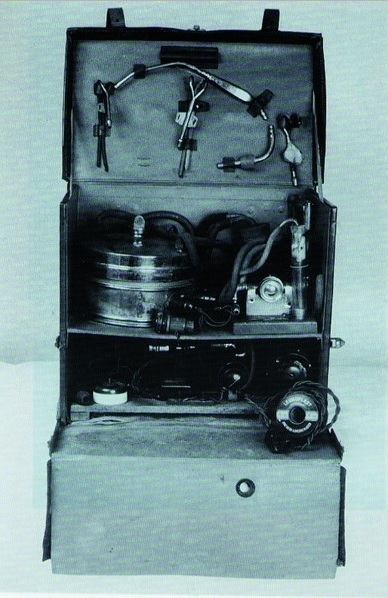
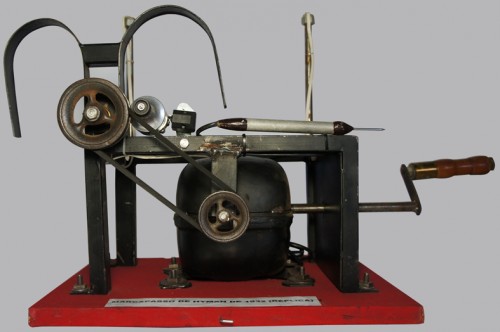
During intracardiac therapy for cardiac arrest, Albert Hyman from the New York Hospital Beth David noted that the success of this procedure does not depend on the medication used, but is caused by the injection of the needle into the heart. He concluded that when cardiac arrest his electrodynamic balance could be disturbed by one injection, which could lead to myocardial infarction. A few shots could improve the situation, but this is too dangerous.Since mechanical stimuli acted due to changes in electrical potential, Hyman came to the idea of direct stimulation of the myocardium by electrical impulses passing through needle-shaped electrodes, with repeated stimulation without any risk. Then Hyman created in 1932 a pacemaker with an innovative design for the time. It consisted of a magnetoelectric generator, which was required to obtain direct current feeding the electrodes. Two large U-shaped magnets applied the necessary magnetic flux to induce a current in the generator. An interrupting disk was used to control the duration of the electrical pulse applied to the electrodes. Such a portable device weighed 7.2 kilograms.
Modern researchers who experimented with Hyman's pacemaker have concluded that it is ineffective due to the low output voltage of the generated pulses, and Hyman himself acknowledged the shortcomings of his pacemaker.
After 1945: Johns Hopps pacemaker
 A few years after World War II, interest in artificial cardiac pacemakers in cardiac practice was reanimated through the efforts of Callaghan, Bigelow, and Hopps from Toronto in Canada. In the course of their studies of general hypothermia, they noticed that with the supercooling of the body, the probability of heart failure is high.
A few years after World War II, interest in artificial cardiac pacemakers in cardiac practice was reanimated through the efforts of Callaghan, Bigelow, and Hopps from Toronto in Canada. In the course of their studies of general hypothermia, they noticed that with the supercooling of the body, the probability of heart failure is high.Heart rate control is crucial for survival during the warming period, when metabolism in the body is accelerated, and for this purpose, engineer John Hopps from the National Research Council of Canada created an artificial pacemaker that can produce the desired rhythm through electrodes after carrying out thoracotomy . The device has been successfully tested on four dogs that suffered from cardiac arrest due to hypothermia.
After successful tests, Hopps realized that such a pacemaker can be used equally effectively to control the pulse at normal body temperature. The device successfully monitored the heart rate in animals at normal temperature, but failed in human tests. Patients suddenly deteriorated due to a violation of the electrical impulse from the atria to the ventricles after myocardial infarction. Most likely, the reason for the failure lies in the fact that the pacemaker was single-chamber: only the atria were stimulated, not the ventricles.
Zolla's pacemaker and first clinical application
 The first clinical use of a pacemaker occurred in 1952. This happened during the reception of a 75-year-old man, when he was admitted to the hospital of Beth-Izreel. After two syncope caused by a sharp decrease in cardiac output and cerebral ischemia due to a heart rhythm disorder, he suffered from a heart block for two years. In the hospital, his condition worsened - he continued to experience attacks of ventricular asystole , despite 34 intracardiac injections of adrenaline for 4 hours.
The first clinical use of a pacemaker occurred in 1952. This happened during the reception of a 75-year-old man, when he was admitted to the hospital of Beth-Izreel. After two syncope caused by a sharp decrease in cardiac output and cerebral ischemia due to a heart rhythm disorder, he suffered from a heart block for two years. In the hospital, his condition worsened - he continued to experience attacks of ventricular asystole , despite 34 intracardiac injections of adrenaline for 4 hours.Dr. Paul Maurice Zol (Paul M. Zoll), the attending physician, applied external electrical stimulation to his patient and successfully stimulated the functioning of his heart for the next 25 minutes. Unfortunately, the patient developed a cardiac tamponade due to multiple intracardiac injections and resuscitation did not help.
Subsequently, Zoll was able to successfully adjust the heart rate of another 65-year-old man with similar attacks of ventricular asystole due to a five-day external electrical stimulation procedure. At the end of the fifth day of therapy, the patient reached an accelerated idioventricular rhythm of 44 beats per minute, and he was discharged.
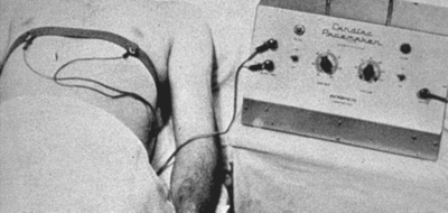
In his work, published in 1952, Zoll described cardiac resuscitation using electrodes on a bare chest with pulses of 2 ms at a voltage in the range of 100-150 volts on the chest to 60 beats per minute. This initial clinical description was the impetus for a comprehensive assessment of cardiac pacing. Doctors and the public acknowledged the fact that heart disease can be defeated by pacing. Zolla's work served as the basis for future research and development.
Mid-1950s: the Lilleichay method
 In the mid-50s, when doctors first began performing open-heart surgery, postoperative heart block turned out to be a particularly serious problem for cardiac surgeons. External electrical stimulation could not be used for patients with this disease, as continuous stimulation is needed for a long time. Heart surgeon Clarence Walton Lillehei (Clarence Walton Lillehei) and his colleagues working at the University of Minnesota medical school, began to develop a better system. They were assisted by engineers from Medtronic , which later became one of the most famous companies in the world in the field of creating pacemaking technologies.
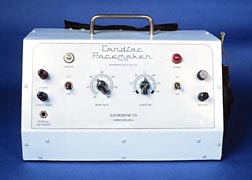
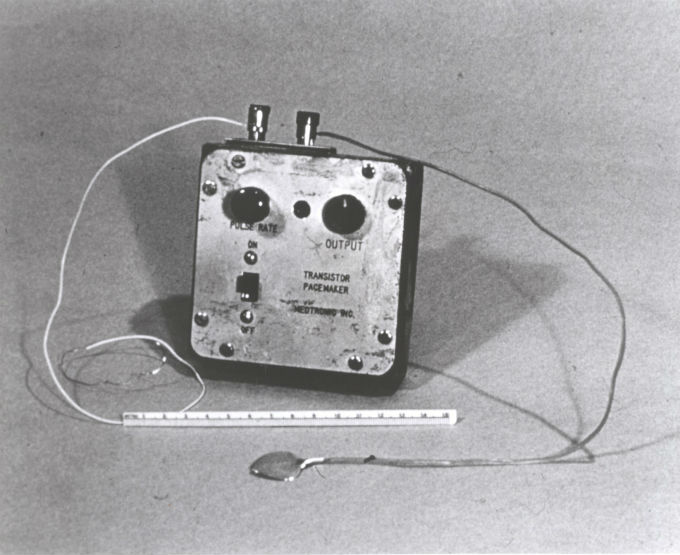
In the mid-50s, when doctors first began performing open-heart surgery, postoperative heart block turned out to be a particularly serious problem for cardiac surgeons. External electrical stimulation could not be used for patients with this disease, as continuous stimulation is needed for a long time. Heart surgeon Clarence Walton Lillehei (Clarence Walton Lillehei) and his colleagues working at the University of Minnesota medical school, began to develop a better system. They were assisted by engineers from Medtronic , which later became one of the most famous companies in the world in the field of creating pacemaking technologies.By 1957, researchers had discovered that by combining a pulse generator with wire electrodes attached directly to a dog's heart, one could control the heart rate. So Lillehai and his team presented the world's first transistor pacemaker.
On January 30, 1957, Lillehai used this technique to restore the heart rhythm of a child with heart block. He underwent an operation to correct the ventricular septal defect. The heart was activated by pulses with a duration of 2 ms at a voltage of 1.5 to 4.5 volts, which is significantly less than in the experiments described by Zoll. In this case, the method was effective and well tolerated by patients.
1958: Oke Senning and Rune Elmquist - the birth of implantable pacemakers
The pacing method developed by Lilleichay could not be sustained for a long time due to the risk of infection, caused discomfort when wearing a pacemaker and became ineffective after several months. The only way to prevent infection - to remove the wires from the body through skin incisions - was the impetus for the development of implantable pacemakers.
 The first attempts were undertaken by surgeon Oke Senning (Ake Senning) and engineer Rune Elmqvist (Rune Elmqvist) at the Karolinska University Hospital in Sweden. The first pacemaker was implanted on October 8, 1958, to 43-year-old Arne Larsson with complete heart block and Morgagni-Adams-Stokes syndrome. The operation was successful, but three hours after implantation, the pacemaker broke down. A similar unit was implanted the next day, but it did not work. Finally, it was decided to abandon pacing for this patient until more successful counterparts are developed.
The first attempts were undertaken by surgeon Oke Senning (Ake Senning) and engineer Rune Elmqvist (Rune Elmqvist) at the Karolinska University Hospital in Sweden. The first pacemaker was implanted on October 8, 1958, to 43-year-old Arne Larsson with complete heart block and Morgagni-Adams-Stokes syndrome. The operation was successful, but three hours after implantation, the pacemaker broke down. A similar unit was implanted the next day, but it did not work. Finally, it was decided to abandon pacing for this patient until more successful counterparts are developed.Fortunately, Morgagni-Adams-Stokes attacks no longer disturbed the patient for the next three years, until he received a second implant. In the end, he underwent 24 surgical interventions and lived until 2001, when he died at the age of 86 from an unrelated malignant tumor.
These attempts to create an implantable pacemaker have played a significant role in the creation of devices on an industrial scale at a reasonable price. Developments in this area were well funded. The first production of pacemakers began in 1970.
1970: upgrade of implantable pacemakers

At the very beginning of the 70s, manufacturers were deeply thinking about using nuclear energy to power pacemakers. The devices used the decay energy of plutonium-238, which was converted into electrical energy. Despite its truly long service life of 10 to 20 years and 99% reliability, the effects of radiation overlapped all the advantages. Scientists have not recommended the use of nuclear energy to power pacemakers, and ultimately such devices are not widely recognized.
During the period of explosive growth of technological innovations in 1973-1980, the pacemakers that were produced in 1970 were quickly outdated. Manufacturers have focused their interest in improving the power source used in pacemakers. The power supply is important because it determines durability and reliability in combination with the type of battery that will be used later, the weight and volume of the pacemaker. After several unsuccessful experiments with nickel-cadmium and mercury-zinc batteries, the lithium battery was adopted as a relatively durable power source.
In addition to ensuring the lifetime of the pacemaker, lithium-ion batteries have allowed for the impulse generators to be sealed. This power source developed over the years to come as the preferred alternative battery for implantable pacemakers.
Programmable and integrated circuits
The first attempts in the direction of programmability, that is, modifications of the implanted stimulator to work non-invasively were made in 1931. The General Electric Company manufactured a pacemaker whose pulse speed was changed by a bistable magnetic switch. The patient could choose between a rate of 70 beats per minute at rest or 100 beats per minute during physical activity by changing the switch with an external magnet. After that, attempts to program the pacemaker were not undertaken until 1972, when Medtronic introduced a programmable device with gear wheels attached to small bar magnets inside an implantable pulse generator.
In 1973, the company introduced another pacemaker, where the speed can be changed by radio frequency signals transmitted through the programmer. Shortly thereafter, programmability became an essential feature of implantable pacemakers.
In addition, the hybrid circuit uses less battery power because it uses it only when performing actions such as opening or closing a switch. The hybrid scheme also allowed manufacturers to reduce their generators and ensure the reliability and durability of pacemakers.
1980s: two-chamber pacemakers
By this time, almost everyone relied on hybrid integrated circuit and lithium battery pacemakers, which would reliably control the heartbeat for at least 8 years. Since 1983, some manufacturers of pacemakers in the United States have begun to compete in the new technological arena of dual-chamber cardiac pacing. Unlike single-chamber pacemakers, dual-chamber stimulate simultaneously two zones: the ventricles and the atria.
Manufacturers and doctors claimed that dual chamber pacemakers provide more effective coordination between atrial and ventricular contractions and closer emulation with the natural heartbeat and gives a noticeable physiological effect. Despite all the advantages, it was difficult for doctors to understand new devices and get used to new indicators: pulse rate, amplitude and duration. Two-chamber pacemakers were more expensive than single-chamber pacemakers, which in 1989 still owned 75% of the market for pacemakers in the United States.
1990s: pacemaker implant boom
 The exact number of operations for implantation of pacemakers in this decade is difficult to name: in 1997 alone, the range varies from 192 thousand to 317 thousand implantations. Violent growth for several reasons. First, between 1990-1999, the number of elderly people with a high risk of cardiac arrhythmia increased. Secondly, cardiologists have learned how to quickly and accurately identify the first symptoms of bradycardia and ECG and were able to schedule an operation in time. And, finally, a new invasive radiofrequency catheter ablation method slightly increased the number of implantations. During this period, doctors have clearly perceived pacemaker as a necessary device for the treatment of heart disease.
The exact number of operations for implantation of pacemakers in this decade is difficult to name: in 1997 alone, the range varies from 192 thousand to 317 thousand implantations. Violent growth for several reasons. First, between 1990-1999, the number of elderly people with a high risk of cardiac arrhythmia increased. Secondly, cardiologists have learned how to quickly and accurately identify the first symptoms of bradycardia and ECG and were able to schedule an operation in time. And, finally, a new invasive radiofrequency catheter ablation method slightly increased the number of implantations. During this period, doctors have clearly perceived pacemaker as a necessary device for the treatment of heart disease.Present tense
Today, a pacemaker is a sophisticated electronic device that consists of three main components: a titanium shell, an electronic circuit, and a lithium-ion battery that lasts from 5 to 10 years. Modern technology allows you to create pacemakers the size of men's watches.
 The implantation of a pacemaker occurs in several stages. First, the heart surgeon makes an incision and highlights one of the veins or arteries — most often it is the lateral vein of the arm or the subclavian artery. Then, one or several electrodes are inserted through the vein into the heart and the correctness of the location of the electrodes is checked using an outdoor unit of the software-hardware complex. Finally, the device itself is placed in the subcutaneous pocket, connected to the electrodes, and then the incision is sutured.
The implantation of a pacemaker occurs in several stages. First, the heart surgeon makes an incision and highlights one of the veins or arteries — most often it is the lateral vein of the arm or the subclavian artery. Then, one or several electrodes are inserted through the vein into the heart and the correctness of the location of the electrodes is checked using an outdoor unit of the software-hardware complex. Finally, the device itself is placed in the subcutaneous pocket, connected to the electrodes, and then the incision is sutured.Source: https://habr.com/ru/post/400047/
All Articles