History of vision correction operations: comparison of risks and side effects
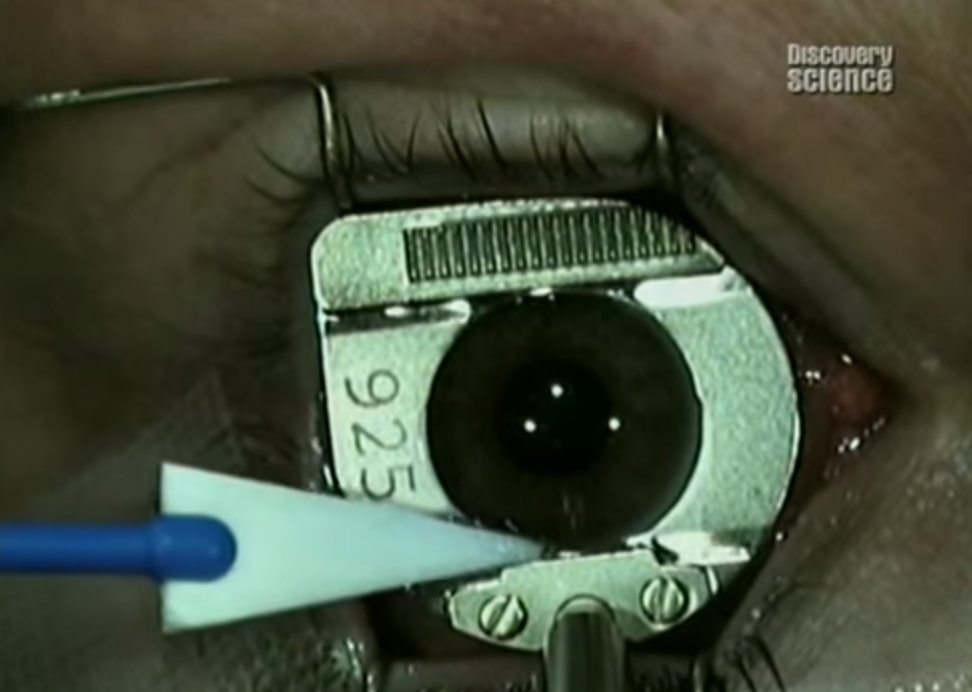
Mechanical device, firing or slowly moving the blade to cut off the upper part of the cornea
Let's start with the story so that it is clear how the methods have evolved, and then we turn to the risks and side effects of modern operations.
So, Dr. Snellen, who invented the eye test table, advanced the theory that you can “scratch” the eye so that the curvature of the cornea changes. This happened in 1869 (in the same year, the periodic table appeared and the Suez Canal was dug up), so they could only scratch with a metal scalpel. Ophthalmology as a separate science was not officially available, and ordinary surgeons were engaged in it - the same ones who cheerfully sawed off hands and feet when an infection occurred.
')
At first they didn’t dare to approach the eyes: the patient seems to be alive, moving and not screaming, which means that there is no sufficient reason to touch him. Therefore, the first vision correction operation was performed by Dr. Lance in Holland only 30 years later, in 1898.
The next distinguished character was an outstanding Soviet surgeon Academician Svetoslav Nikolaevich Fedorov, who proposed a very peculiar method: to heat the cornea of the eye to the point until it is deformed. But along with Sato, a Japanese ophthalmologist, they quickly moved on to the cuts. Sato cut from the inside and thus created many complications, and Fedorov made notches with a diamond knife outside. These very cuts actually marked the beginning of modern laser operations.
Scalpel
It must be said that ophthalmology as a separate specialty appeared in Germany in the middle of the nineteenth century (1857), when the German society of ophthalmologists was born. In the United States, for example, until the 50s of the twentieth century, this was called the “ophthalmology section” and was located in the department of general surgery.
SN Fedorov from the USSR, Sato from Japan and Rousy from the USA in the 80s came to similar conclusions. First, they heated the cornea to the desired stage of deformity and watched what would happen to the patient's optics. The patient's cornea cooled, he calmed down, he saw well, but after a while the effect disappeared. Therefore, the branch was declared unsuccessful, and surgeons took up the incisions. More precisely, the real push appeared when they began to make notches on the cornea. The idea was Sato, but his results were predictably bad.

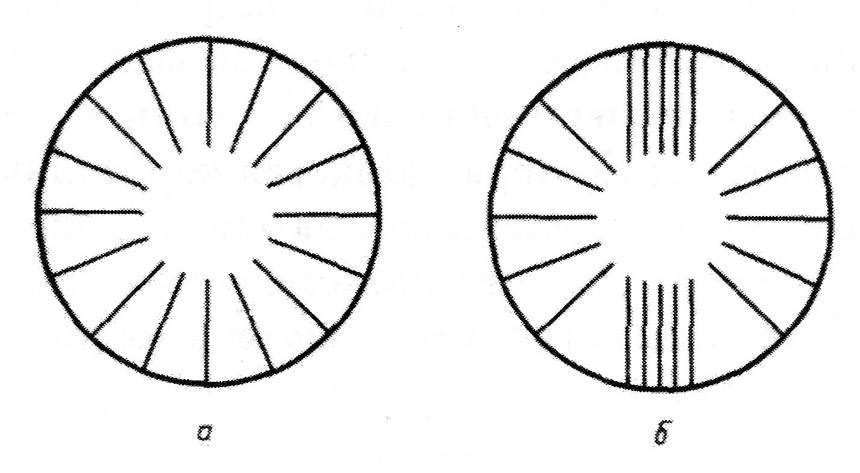
Sato first did notches from the inside up, that is, he got access to the inner (lower) part of the cornea of the eye and cut through the endothelium - the lower layer of the cornea. The endothelium predictably did not regenerate, the corneas became muddy. Then, as a result of the experiments, a method of incisions on the surface quickly appeared through the epithelium and the bowman's membrane directly into the stroma. In 1972, Academician S.N. Fedorov published a systematic scientific work, where he described the methods of operation and the mechanics of various sections. Up to this point randomness reigned in the field - everyone did, relying only on his own poor experience and not really understanding the architecture of the eye. Diagnostics - by hand, depth of cut - intuitively, the number of notches - depending on the size of the doctor’s fingers. S.N. Fedorov called the operation radial keratotomy. It gained popularity in the USSR and the USA, as well as in Latin America. The Lindstrom version soon appeared - the so-called mini-CT, a little less invasive.
In the USSR, they began to do it en masse, in Colombia and the USA too. There were almost no followers in Western Europe due to conservatism.
The technology of applying the notches themselves changed insignificantly: S.N. Fedorov's theory worked perfectly, except that the tools became a little more precise - the metal scalpels were replaced with diamond ones.
After 10 years, gained clinical experience. And the first ten-year study on the George Waring Third RCT came out - he was able to show that the RCT works well, but hypermetropization occurs: people become more farsighted over time. Walter Sekundo, by the way, communicated with him and with Russian surgeons when he developed his own laser correction technique and said that it was in the USSR that surgeons got a lot of experience in treating such complications because they were very often met (thanks to the mass operations, they made more million).
Excimer laser
Then came the first infrared excimer laser. It is believed that it was first used by Steve Torkel, who invented how to use an industrial laser in medicine. Due to the fact that all changes of refraction were made at that time with a cut, he decided to simply replace the metal scalpel with a diamond, and a diamond with an even more accurate one - with a laser. Yes, yes, it was then done manually by a laser machine, in fact.
Began to experience - it turned out that the laser on special guides allows you to achieve much greater accuracy than manual cut. And the era of automation of refractive surgery operations began.
The problems were that the excimer lasers were heating the cornea, and it was just overgrown at the incision sites. Radial correction works in such a way that you weaken the mechanics of the cornea by incising, evaporating or withdrawing from it a part of the collagen fibers. Then it sags in the middle and closes. Then they came from the middle with an "asterisk", the cornea became flatter. There are different methods - we found patients with “only 16 incisions” with laser correction, and there are those who have 32 incisions. At MNTK, they then created an actual conveyor belt, where people moved in a circle, and each surgeon did a single stage of the operation.
Dr. Marguerite MacDonald (by the way, she was probably over 75 years old, because she taught Walter in the late 80s at the department of Louisiana State University in New Orleans) in 1985, she first performed an operation called photorefractive keratectomy (PRK). She decided to use the laser, rather, as a grinding tool (according to the method of Srinivazan and Brenin, described in 1983, but not tested). During the operation, the patient was “stolen” by a part of the cornea. In the center of the cornea a lot of tissue was evaporated, further to the edges - a little less. It turned out that the lens, which is formed by the cornea, changed its optical properties.
PRK principle
The problems at that time were that the working area of the laser was chosen about 4 millimeters - they did not go further to the edges. And the pupil of a healthy person opens up in the dark sometimes up to 6–8 millimeters, that is, right in front of the pupil there is a ring formed by a cut. Hence, strong halo effects, that is, a very interesting image of any light sources at night. In general, patients at night were, if not helpless, then close to this state: the light of a car traveling towards me deprived them of their ability to navigate.
In the 90s they began to produce lasers in large quantities, and then quickly expanded the working area. Since then, PRK has not changed much - today this technique is still alive (why - below), but it is performed with more modern devices and wide ablation zones, less traumatic. But if you decide on this operation - remember that it simply destroys the Bowman's membrane. But, it must be admitted, in some cases this is a completely acceptable loss.
Lasik
At about the same time as the PRK, the idea was to not evaporate the lens on the surface of the eye by “grinding”, but to remove the top layer of the cornea, cut the cavity under it, and then sew the top layer back. Actually, at first Dr. Seiler from Berlin, who worked with opacities and superficial scars, invented the FTC operation using an excimer laser (the grandfather-guru of ophthalmology, Theo Seiler, by the way, still treats in Zurich, he has his own clinic). Based on his practical developments and the theory of Hosse Barracker from the 50s, Dr. Ioannis Pollikaris from the warm island of Crete came up with a practical embodiment of this method.
Hosse Barracker, I must say, was an extraordinary person. In the year 49, before the lasers, before systematization and before the advent of the normal methodology, he simply put the patient to sleep, cut off the surface of the cornea of his first eye, quickly frozen, drove to the other end of the city, polished this piece of ice as it should in the jewelry industry, and then drove back in the operating room. By the time of arrival, the cornea melted, and he had already converted the part sewn back to the patient. Actually, omitting the trip to the other end of the city and the general romance of the 50s, we even found in 92–93 exactly such keratomelosis operations. Of course, the system was more modern - they made the first cut to lift the “cap” on one patch, then the second cut, and then the “cap” was sewn back.
But let us return to Pollikaris, the charming doctor Barracker and the calm and quiet Lucio Buratto (he is also a grandfather-guru who lives in Milan for his pleasure and "works" to the fullest). They all suffered from the fact that such a good method gives a not very accurate correction - the average surgeon's spread was plus or minus three diopters (therefore, it was used only for patients with really severe myopia). Using the method of Jose Barracker, Ioannis Pollicariz and Lucio Buratto realized that an excimer laser allows you to grind the cornea more accurately than to cut it off with a blade.
As stAndrew noted in the commentary: “They cut the flap with a knife. It is rather psychologically very unpleasant when you put a shaybochka on your eye, which buzzes and cuts the eyeball of the eye on the living. Now flap do femtosecond laser. "
By the way, this "shaybochka" is in the picture at the top of the post.
This is how the LASIK procedure appeared (this is an abbreviation: K is keratomlilosis, the other letters are laser assisted, that is, "with the support of a laser"). Pollikaris brought the most progressive part into the operation - he left the “leg” or “loop” for the “cap”, that is, he allowed to put it back relatively evenly, and so that she had something to hold on to. By the way, speaking of the flap shift with LASIK and femtoLASIK, it is worth remembering about this main problem. The cut off “lid” rests precisely on a flap about 20–40 degrees wide, and is covered with epithelium from above. And the fact that it stands still, and not “bounces off”, is provided by the epithelium. And nothing more. Therefore, with eye injuries, it can “lay back."
In 1992, LASIK was introduced as a mass operation.

Lasik
FemtoLASIK and FLEX
Surgeons wanted from a laser more accurate cutting and less heating of the tissue. That is a much higher frequency at a much lower pulse energy. When the first femtosecond lasers appeared (modern ones give an impulse tens of thousands of times shorter than the first generation), the rush around them immediately began.
And for good reason. Initially, FemtoLASIK was developed - all the same good old method of the charming and ingenious Barracker, but with much greater precision and without any special surprises. It was a wonderful operation, and it worked like a clock. Actually, it works now.
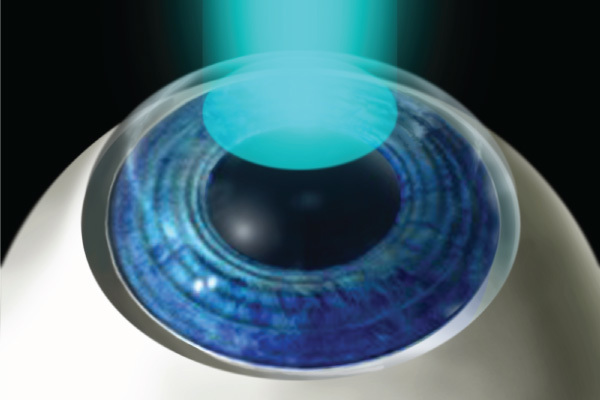
With the help of a femtosecond laser, a horizontal incision is made (what was previously done by an eyeglass with a moving steel blade), then the patient is transferred under an excimer laser, a lens is placed inside the cornea stroma, and the first one is cut off.
How the laser works, I already wrote here .
But the laser made it possible to do something that did not work out earlier, namely, not “punching” the surface of the cornea of the eye, to cut inside, forming a cut that may not touch the surface at all. This is how FLEX appeared - in fact, it is neither better nor worse than femtoLASIK, since there is still a flap there - a “flap on the leg”. But FLEX was already done by one laser, not two, so the operation took place much faster, and the smell of the “burning cornea”, which is typical for an excimer, was not. And the cut on the lens was curvilinear, which for 2006 was a breakthrough. However, because of the high accuracy of the cut (or rather, small thickness), sometimes there were adhesions that had to be carefully separated. The lasers of that time only provided the necessary frequency, and therefore besides the adhesions, bridges could appear as a result of inaccurate focusing (due to fat microdroplets, for example, on the surface of the eye), they also had to be separated with a spatula.
Since we live in the world of patents, competitors Zeiss (manufacturer of lasers) began to urgently invent their own analogues. A very good evolutionary branch was the story of superLASIK, which was made on a special wavefront-map of the eye. All distortions are measured and transmitted to the firmware, which builds an individual profile.
The downside is that part of the distortion gives the cornea (it can be adjusted), and some - the lens. It is more difficult with him - he grows all his life, and all the advantages of the operation can be leveled in 5 or 10 years. In modern operations, the principle of an aspherical lens on the cornea is used — it is done in such a way as to “show” as well as possible in as many years. Modern optimized profiles for spherical aberrations (namely, they most of all create problems like “I see badly at night”) produce better results or on a level with lasers that do not have aspherical profiles, but they solve the problem on individual profiles. If you have a Zeiss laser MEL-90 or “VISX STAR S4” from AMO, then they allow both. At the end of the operation there is almost no difference.
Hence the myths about the "3000 individual lenses in the cornea" and so on. Zeiss updated the mathematics on his new generation of lasers, and now it is extremely difficult to catch up with him - in at least two years of clinical research his standard aspherical profiles are better or not worse than those specially designed for a specific operation on other lasers. Now the latter are catching up, since more difficult preparation of the patient is needed in order to achieve the same result.
The next stage of working with the mechanics of the cornea - FLEX. This is all the same good old keratomylosis, but at a different level of accuracy. Then, for FLEX, they began to make a cut not in the full arc, but in half, and then Professor Walter Sekundo and Markus Blum decided to try to cut the lens inside completely and get it through a small cut.
SMILE
So FLEX evolved to SMILE - this is also an abbreviation, which means "minimally invasive lenticular extraction." That is, cutting the lens inside the eye with its subsequent getting.
How exactly this happens, you can look here (I was asked to warn several times, so it’s better, probably, not to watch the link for food, although there really isn’t any harm there).
In 2007, my partner, Professor Walter Sekundo, made the first SMILE, then with two more cuts of 5 millimeters - it was assumed that the second was needed so that when washing the cavity of the lenticle in the stroma, the liquid could freely exit. Two to five is 10, not 20, as was done for FLEX or femtoLASIK, which means that there were much more nerves inside the eye and a much less injured bowman membrane.
Pretty quickly managed to reduce the incisions to 2.5 millimeters. And then Walter Shaur’s colleague from India, Rupal Sha, proved that only one was enough. Today, most experienced surgeons work from 2 to 3 millimeters (but most Russian surgeons from 3 to 4.5 mm).
ICL
If FemtoLASIK and SMILE perfectly solve the problems of myopia, then with long-sightedness or more complex effects is not so easy. But having the ability to cut lenticules inside the eye, you can use not only the effect of stroma collapsing and the formation of a new lens shape. You can insert into this cavity something new and interesting. The same tireless Soviet surgeon Academician S.N. Fedorov invented an operation (in the future it was called ICL - an implantable contact lens). He inserted the lens or in the back of the eye, or in front of the lens - the benefit of the operation on implantation of the lens was already well mastered. But Academician S.N. Fedorov did not have modern materials; therefore, every fourth patient received an unpleasant side effect: due to the deterioration of the nutrition of his own crystalline lens, his clouding began.
In the US, a new copolymer was created - partly silicone, partly a pig. More precisely, they used pork collagen. From 25% of side cataracts managed to leave up to 3%. The operation became widespread, and a mass of improvement branches began. Dozens of models appeared and disappeared due to complications. Since those years, manufacturers have changed their name a couple of times, but 90% of the market is still the same "half piggy." Although, of course, the lenses are now made flexible to introduce them through a small incision.
Today, a stable operation of this kind has been developed by Jan Vorst from Holland - he has a lens with “claws”, it hooks on the iris and is held in the front chamber. Professor Sekundo, by the way, specifically went to Jan Vorst in Holland to learn and understand the technology of manufacturing at the Ophtech factory, which Vorst Jr. now leads.
What is being done today in Russia and in the world
In Germany, according to Professor Walter Sekundo, who has access to the commercial information of the German network of clinics, the situation 5 years ago was as follows:
- PRK for rare indications and for cities where there is no separate ophthalmology (“As we joke, the PRK operation is very simple, even a cat can master it with proper assistance,” says Professor Sekundo).
- LASIK for those who do not have money for femtoLASIK.
- FemtoLASIK and its derivatives for standard cases.
- SMILE for those who are willing to reduce the risks for an additional fee (as a VIP surgery with experienced surgeons).
Over the next 2 years, SMILE began to be made about as often as femtoLASIK.
To date, the situation has changed somewhat. The fact is that due to the increase in the laser frequency and the improvement of the energy parameters, the accuracy of SMILE became significantly higher, and 2–3 years ago it became equal to femtoLASIK on corrections from –2 (on smaller femtoLASIK it is more accurate, and PRK is ideal in accuracy for –1) . There remains the question of high prices, and little will change here because only Zeiss knows how to do the necessary optics for the time being. A single laser switch for SMILE operation for one eye costs 300 euros.
Now in Germany on the same network, this is what happened:
- PRK keeps around 7–10% (thin cornea, a number of difficult cases, small corrections of about –1 diopters, plus the advertisement “no one will even touch you,” a huge clinical practice).
- Regular LASIK even patients feel almost barbaric, and it is no longer there.
- Then the most popular is femtoLASIK with analogues, about 10% of operations.
- FLEX - units per year, since this is an unnecessary evolutionary stage.
- And then - SMILE, its about 80%.
FemtoLASIK is likely to drop to 5–7%, as well as PRK. It has two advantages: firstly, there is less evacuated tissue compared to SMILE with a small correction, because the lenticule must have at least 30 microns to grab it. Secondly, after it a sharp vision appears faster - it is a day or two, not 4 days, or even a week. For some, this is important.
In Russia, the situation is a bit worse: LASIK is still being made due to low prices (the equipment for this operation costs from 50 to 80 thousand euros, and the operating room with the VisuMax Carl Zeiss femtolaser - half a million euros). SMILE is fairly rare. The problem is in the high price and, as a result, the small experience of surgeons - for example, some colleagues have more than 20 thousand FemtoLASIK operations on all their surgeons, but only a few or tens of them have SMILE. The problem is that, as was the case in one German headline, "In refractive surgery, you need a surgeon again." That is, you have to do something with your hands, and the frames that were prepared for LASIK do nothing with your hands. Hence the question of qualification. And dropouts - there are many where in the world SMILE's reputation was spoiled a bit by surgeons who were not very well able to work manually. Therefore, if you are discouraged from this method in the clinic - it is better to obey, most likely, they do not want to risk knowing their surgeon. Many surgeons are afraid of new, because they are afraid of complications. This is a normal human property: leave everything as it was before.
By the way, LASIK will live on our market for a long time, if only because the old lasers from Europe are leaving not only the third world countries, but also to Russia, and they “settle” in low-cost hospitals.
- I have done femtoLASIK, FLEX, superLASIK or PRK for a long time ... did not you have to?
If you made PRK for the price, and not according to indications, you do not have a Bowman's membrane, and this really was not the best idea. However, as long as you do not have problems with intraocular pressure, the risks are very low. PRK is a good operation with a 20-year history, and it was made exactly with high quality. Because there it is very, very difficult to make a mistake at the moment of the operation itself.
If you have done femtoLASIK or its analogs, several years have passed and there are no problems - congratulations, most likely, there will be no problems anymore - the risk for the next 20 years is only about 1-2%.
If you are going to make a correction and choose between SMILE and femtoLASIK not because of the financial component, then SMILE is slightly better. However, now in Russia, if you are going to do femtoLASIK - know that a sensible surgeon will be able to do this operation with a minimum of risks, the technology itself has been worked out, experts in the world know it perfectly, prices are generally earthly. A few years ago, I personally made a laser correction for both my mother and daughter, and many of my colleagues did laser correction for themselves and their loved ones.
And there is SMILE. This reduction in the probability of side effects, roughly speaking, from 2-5% to 0.5%. And both naturally reversible and irreversible. The Bowman's membrane is minimally injured, many nerves remain that would have been destroyed with other methods of correction. But it is more expensive and requires the skills of a surgeon. If you trust a doctor and are willing to pay to reduce the risk of irreversible complications, the choice is fairly obvious.
In the next post there will be answers to all your remaining questions, in detail about the course of the operation, protection of the laser from various kinds of emergency, interruptions of the operation and a story about the device of the eye at the micro level, so that it is clear how the regenerative processes proceed. A little later, I will tell you about the world and Russian clinics that are worth paying attention to.
Source: https://habr.com/ru/post/399871/
All Articles