History of rare neurodegenerative diseases

Neurodegenerative diseases - a group of slowly progressive diseases affecting the work of the nervous system. Some are more common, others - less. They may be inherited or acquired. Some of them are treatable, but for others they have not yet invented drugs.
Today we will talk about two rare neurodegenerative diseases - kuru disease and fatal familial insomnia (FFI) . From the first, a whole tribe in Papua New Guinea suffered in its time, the second still does not give rest to one Italian family. At first glance, these diseases have nothing in common, but as is usually the case in life, in fact, everything is not so straightforward.
')
Kuru disease
Until the 1930s, almost no one in the world knew whether anyone lived in the highlands of Papua New Guinea. The society remained in the dark until Australian gold miners explored the terrain and discovered about a million people.
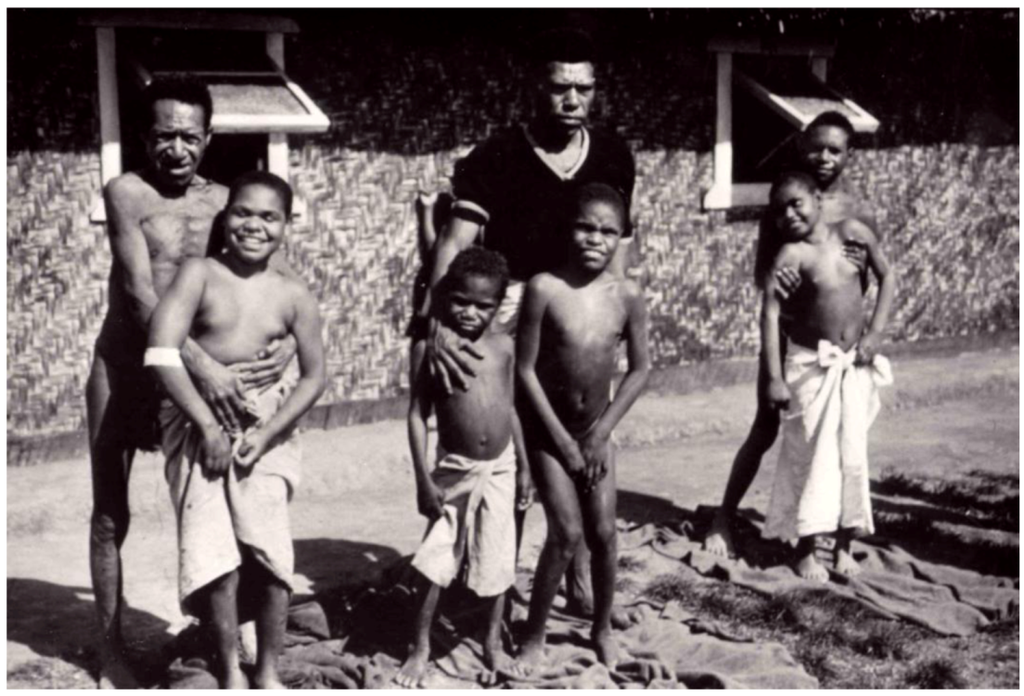
The first researchers went to this area in the 1950s, and immediately found something disturbing. In the Fore tribe of about 11,000 people, 2% of the population died each year from a disease unknown to science. Tribal residents called it "kuru", which means "trembling" or "spoilage."
Locals knew: if the first symptoms appeared, then death is inevitable. At first, patients had difficulty walking, which further led to a complete loss of control over the limbs. They also lost the ability to manage their emotions. For this reason, some publications that later wrote about the disease called it a “laughing death”. A year later, the patients could no longer get up from the floor, eat and control their body on their own. This disease was described in detail in 1957 by two doctors: Daniel Carlton Hajduzek and Vincent Zygas.
Faure were convinced that evil shamans cause kuru. Primarily, the disease affected adult women and children under 8 years of age. Some villages have completely lost young women. Residents were obsessed with trying to save themselves, because they felt that their tribe was on the verge of extinction.
What caused this disease? The answer to this question was not given to scientists for many years. After the scientists checked the terrain and eliminated the effects of pollutants, they decided that the disease was most likely genetic. This was the first major misconception among scientists regarding the nature of the disease. Subsequently, scientists have found that kuru is not a genetic disease, because it affects women and children in the same social groups, but not in genetic ones. For the first time, the kuru appeared in northern villages at the turn of the century, and then moved south for many decades.
After scientists excluded the inheritance of the kuru, they decided that the disease was a manifestation of a slow virus. To confirm this hypothesis, the group came to grips with research.
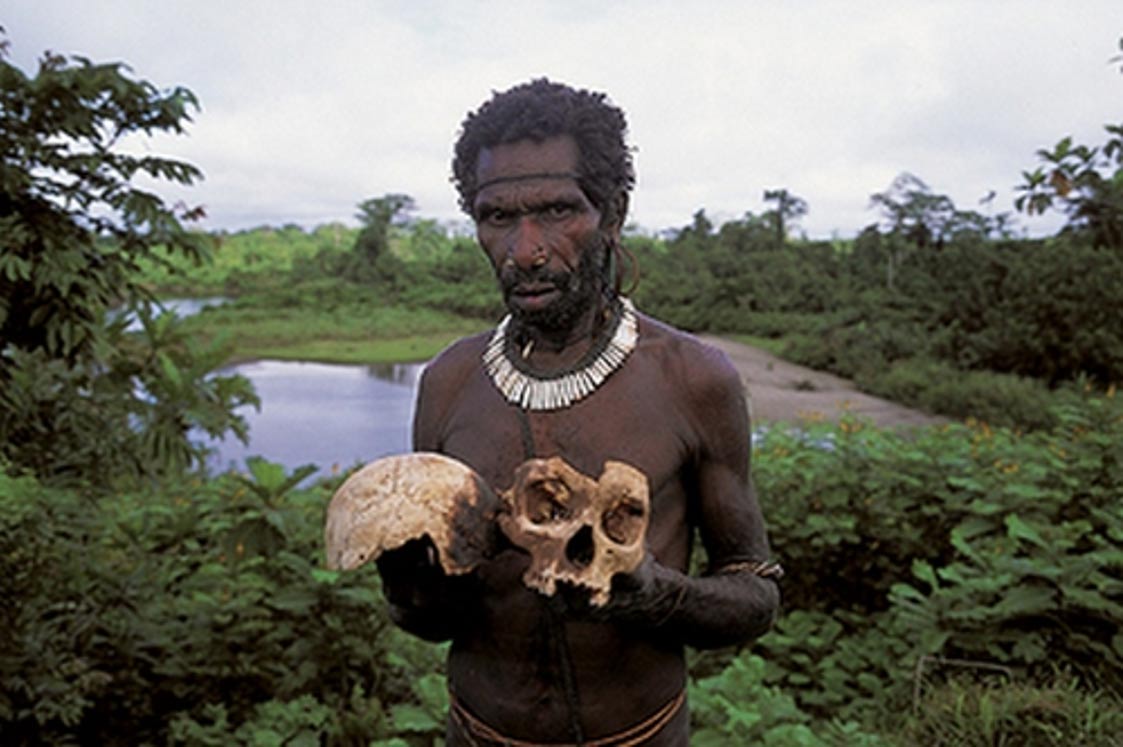
Later, Gaiduzek and Zigas guessed what was happening: the disease was associated with funeral rites adopted by the Faure tribe, namely, the eating of the bodies of the dead. In many villages, when a man died, women removed the brain from the body, mixed it with fern and boiled it in bamboo dishes. The remaining parts of the body were cooked on fire and ate everything except for the gallbladder, as a sign of love and sadness. The ritual involved mostly adult women, because it was believed that their bodies were tamed by a dangerous spirit that would accompany the corpse to another world. Sometimes in honor of the holiday women gave small portions of such food to their children. This explains the mortality among women and children.

However, scientists did not have direct evidence of the theory. Then they conducted an experiment on chimpanzees: they were given materials from the brain of an infected person. The animals showed symptoms of kuru, which made scientists think that the cause was indeed a slow virus with an abnormally long incubation period: in humans it ranged from 2 to 23 years. For the discovery of the infectious nature of Kuru disease, Carlton Haiduzek was awarded the Nobel Prize in Physiology and Medicine in 1976.
Later, his theory was mistaken: the agent for the kuru was not a virus, a bacterium, a fungus, or a parasite — it was a completely new infectious agent for those times that did not have genetic material, could survive boiling and was not alive. As a group of scientists led by Stanley Prusiner later find out, the causative agent of the kuru will be a protein with an abnormal tertiary structure and not containing nucleic acids — prion .
The structure of the prion protein and its replication is fundamental in the study of kuru. Although the exact details regarding the structure of prions were initially unclear, Prusiner put forward three hypotheses. He assumed that these were either viruses, or proteins associated with a small polynucleotide, or proteins lacking nucleic acid. In the course of numerous studies, it was possible to confirm the last hypothesis of the scientist. In 1997, Prizoner received the Nobel Prize for the discovery of prions - a new biological source of infections.
Under normal conditions, these cellular proteins are harmless, but they have the ability to turn into stable structures that cause a number of neurodegenerative diseases, including kuru. Prions “subdue” healthy proteins to their will and turn them into similar ones. Ultimately, this kind of chain reaction leads to the formation of a number of prions, sufficient to kill the bundles of nerve cells of the brain.
These proteins literally turn the cerebellum into a sieve, penetrating it through and through, because the patient loses coordination of movements. They also form tangles that impede the flow of natural processes in the brain. As a rule, a sick kuru goes through three stages. Headache and joint pain are precursors to the disease - common symptoms that patients often do not pay enough attention to. At the first stage, a person with a kuru loses body control, has difficulty in balancing and maintaining posture. At the second stage, or the “sedentary” stage, a person loses the ability to walk. Tremor in the limbs and involuntary twitching. In the third stage, the patient is usually bedridden and unable to control most of the functions of his body. Dementia or behavior change may occur. At the same stage, the patient has difficulty in swallowing and loses the ability to eat in the traditional way. Ultimately, most patients with kuru die from pneumonia.
It is possible to get the chicken only when eating the infected brain or coming into contact with the open wounds or ulcers of the patient, therefore it is not possible to speak about the wide prevalence of this disease. However, it was the study of kuru disease that led to the discovery of prions that cause a number of other neurodegenerative diseases: fatal familial insomnia, Creutzfeldt-Jakob disease , Gerstmann-Straussler-Sheinker syndrome, and others.
Unfortunately, it is not possible to cure chicken. Prions that cause this disease are difficult to destroy. The brain in which these cellular proteins have worked, remains infectious even if it is stored in formaldehyde for many years. Therefore, in this case, the best medicine is prevention. Thus, in the middle of the 20th century, governments and societies sought to prevent the disease by hindering the social practice of cannibalism. Since the 1950s, the Faure tribe has abandoned its funeral rites, and now the disease has almost completely disappeared. Today, kuru is rarely diagnosed: symptoms similar to kuru are more likely to indicate another serious neurological disorder or spongy disease.
However, research on the disease is still ongoing. In 2009, a group of scientists from the Medical Research Council of the United Kingdom discovered that some people who survived the Kuru epidemic carry the V127 genetic mutation in their body, which gives them a strong resistance to the disease. Perhaps someday scientists will be able to find a cure that can withstand the destructive activity of prions.
Fatal familial insomnia
In 1797, a man named Giacomo was born in a small town near Venice. The members of his family, as a rule, were all on the selection: tall, broad-shouldered and muscular (however, the current generation has retained these attractive features). One day in the fall of 1836, Giacomo collapsed with an inexplicable illness, and began to suffer from dementia. In the end, the disease finally chained him to the bed, where he lay in agony without sleep. Soon after, he passed away.
Giacomo left three children, one of them left behind six more heirs. The next century and a half, his descendants flourished: family members became prominent Italian doctors and businessmen. Their condition would allow them to own 130 apartments in Venice, including the palazzo on the Grand Canal. But in parallel with the high position in society, in the parish books, in front of each family, there was a record of premature death. For decades, they recorded oddities such as epilepsy, fever, fever, accompanied by gastric upset. Later, the death certificates of family members will indicate meningitis, encephalitis, econo, Alzheimer's disease, leukoencephalitis, alcoholic encephalopathy, and other diseases.
In fact, the cause of death in all cases was one - fatal familial insomnia. This genetic disease was not officially defined until 1986. It is so rare that for a long time only the descendants of Giacomo were the only people on the planet affected by this disease. Since then, another 30 families have been found that have undergone fatal family insomnia.
The overall picture of the symptoms looks rather gloomy. The first signs of fatal family insomnia can be found at the age of 32-62 years old, the average age is 51 years. But there were cases when the disease occurred at the age of 18 and at the age of 72. The very first and foremost symptom of the disease is insomnia that progresses with time.
In the first stage, the patient will try to compensate for the lack of sleep with an afternoon nap, but as a rule, he fails. Pupils become tiny, pressure increases. There is severe sweating, in men comes impotence. For about four months he suffers from panic attacks and unexplained phobias.
During the next months of fighting the disease, the patient will try to fall asleep, but each time, closing his eyes, he will reach a maximum of mild stupor, trance. The brain will cease to rest. Panic attacks become more serious, and will last about five more months.
 In the third stage, general insomnia causes rapid weight loss and limitations in mental functioning. This stage lasts about three months. At the last stage, the patient is completely weakened and suffers from dementia and immunity to the world around about six months. Then he is waiting for a coma and death. One of the most tragic aspects of the disease is that despite the fact that the patient shows all the signs of dementia, he clearly understands what is happening to him.
In the third stage, general insomnia causes rapid weight loss and limitations in mental functioning. This stage lasts about three months. At the last stage, the patient is completely weakened and suffers from dementia and immunity to the world around about six months. Then he is waiting for a coma and death. One of the most tragic aspects of the disease is that despite the fact that the patient shows all the signs of dementia, he clearly understands what is happening to him.At least 30 of the descendants of Giacomo have died this way in the last century — 13 since 1973 and another 7 in the last decade. Among the living about 25 people are carriers of the gene that causes this disease. In the area of Venice in Italy, where most of the family still lives, the version that the descendants of Giacomo are cursed has long been widespread. Locals do not cease to discuss the tragic fate of the family, which can not but affect its future existence. Young girls from this family find it difficult to find a partner in life, despite their visual appeal and decent condition. It even goes so far that family members cannot get insurance.
In the mid-1980s, Italian newspapers became interested in the story of Giacomo's descendants. A rich family with an unexplained illness has become exotic. Media attention came at a time when the first reports of a new European scourge appeared - mad cow disease. As it turned out later, both of these diseases unite pathogens - prions.
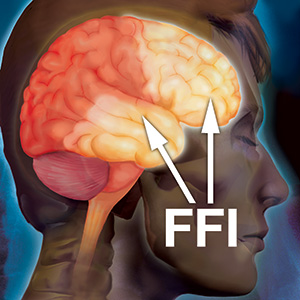
In almost every case, fatal familial insomnia is caused by a mutation in the PRNP gene. This mutation means that in the protein that contains this gene, aspartic acid replaces asparagine at position 178, turning the protein into a prion. But for the occurrence of the disease is not enough. In order for the symptoms of the disease to appear, the amino acid methionine at position 129 of the protein must be present in the prion. Together with amino acids, asparagine and methionine, in these particular positions, normal prions acquire a pathological form.
There are rare cases where the disease is not due to changes in the genes. As of 2016, only 24 such cases were recorded. Here, fatal familial insomnia occurs when some of the normal human prions spontaneously transform into an abnormal form that causes illness and then changes prions in other cells, as is the case with kuru disease.
Prions that take on an abnormal shape cause changes in the thalamus , a region of the brain that is responsible for redistributing information from the senses (except for smell) to the cortex. This same area governs the cycle of sleep and wakefulness, a sense of balance, a sense of pain, aspects of learning, memory, speech, and language understanding. Even emotional experiences and character depend on the thalamus.
When fatal familial insomnia causes a mutation in the PRNP gene, it is inherited in an autosomal dominant fashion. This means that for the occurrence of the disease is enough the presence of one mutant allele in the non-sexual chromosome. In some cases, a person inherits a mutation from an affected parent. In other cases, the disease may occur as a result of new mutations in the genes.
A person with fatal insomnia in 50% of cases passes the gene to his children. Sometimes it happens that a disease is not inherited, provided that the disease is caused by a spontaneous change in prions, and is not caused by genetics.
Like kuru, fatal familial insomnia cannot be cured or slowed down. You can only alleviate the symptoms and create the best possible comfort around the patient.
Source: https://habr.com/ru/post/399813/
All Articles