A link between mitochondrial dysfunction and Alzheimer's disease has been found.
Scientists from the ASU-Banner Research Center for Neurodegenerative Diseases and Biodesign Center for Bioenergy suggest that repairing damaged genes associated with mitochondrial functions will help stop the onset of Alzheimer's disease.
On November 25, 1901, a 51-year-old woman was admitted to a hospital in Frankfurt, demonstrating a bizarre combination of symptoms. Her behavior was unpredictable. On the face all the signs of paranoia, as well as auditory hallucinations, disorientation in space and serious memory impairment. In response to a request to write her name, she displays “Mrs.” and then lingers over the page, unable to remember everything else. “I lost myself,” she will tell her doctor. In time, she withdraws into herself, before her death on April 9, 1906.
')
 The tragic incident of Augusta Deter might have been lost among other medical records if her doctor, Alois Alzheimer, had not conducted a thorough examination of her state of health. In addition, he analyzed the patient's brain tissue after death and found clear amyloid plaques, as well as signs of neurofibrillary tangles. Augusta Deter became the first person diagnosed with Alzheimer's disease.
The tragic incident of Augusta Deter might have been lost among other medical records if her doctor, Alois Alzheimer, had not conducted a thorough examination of her state of health. In addition, he analyzed the patient's brain tissue after death and found clear amyloid plaques, as well as signs of neurofibrillary tangles. Augusta Deter became the first person diagnosed with Alzheimer's disease.Today, society is facing an Alzheimer's disease epidemic: in the United States alone, about 5 million people suffer from it. According to analysts from the Center for Disease Control and Prevention, this number will increase to 14 million by the middle of the century. From the list of the 10 most common diseases leading to death, Alzheimer's disease remains the only one that cannot be prevented, treated or cured.
In their study, Paul Coleman, Diego Mastroeni, and their colleagues at ASU-Banner and Biodesign studied the role of mitochondria in the pathology of Alzheimer's disease. Mitochondria work as cell energy centers and are crucial for health and disease. The work of scientists relies on earlier work, in which gene mutations affecting mitochondrial function are the intended cause of the onset and progression of the disease.
Mitochondria — membrane organelles present in all living organisms — are often called cell power stations. Using a process known as oxidative phosphorylation (OXPHOS), they produce most of the chemical energy of a cell in the form of adenosine triphosphate or ATP. In addition to supplying energy to the cell, mitochondria are involved in cell differentiation and cell death, as well as in their growth and maintenance of the cell cycle.
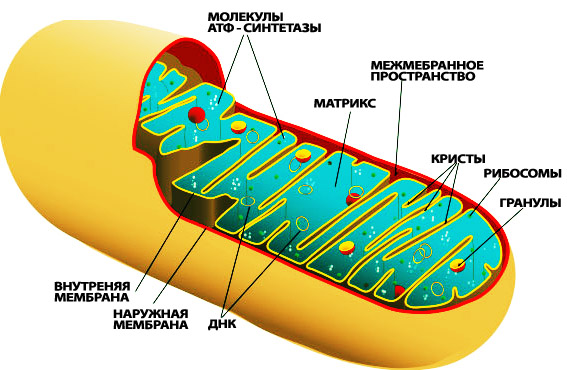
Mitochondrion structure
Mitochondria differ from other cell organoids in that they have their own DNA . It differs from that contained in the cell's nucleus. This became possible due to mitochondrial evolution. These organelles are descended from free-living bacteria, which “colonized” other cells about 2 billion years ago. Being included in cells containing the nucleus, these endosymbionts (organisms living inside another organism and benefiting it) lost most of their natural structure, but retained their own DNA.
Because mitochondria play an important role, mitochondrial dysfunction is associated with a wide range of diseases, including cardiovascular, autism, schizophrenia, bipolar disorder, epilepsy, stroke, diabetes, and various forms of dementia like Alzheimer's disease.
Age-related neurodegenerative diseases such as Alzheimer's disease develop for a long time before they manifest themselves. The earliest physiological and molecular processes are still unknown. The results of the Coleman and Mastroeni laboratories revealed early changes in the encoding of the nucleus (rather than mitochondrial mRNA ), which occur in people after 30 years. “This gives us the opportunity to look where we suspect the earliest cellular changes occur in the progression of Alzheimer's disease,” says Mastroeni.
In this study, tissues from the hippocampus , a part of the brain that plays a crucial role in human memory, were studied. She is the first to be seriously affected by the onset of the disease. Using micrometric analysis, the researchers studied hippocampal tissues of 44 healthy people aged 29 to 99 years, 10 with moderate impairment and 18 with Alzheimer's disease.
The reaction was evaluated from two sets of genes: the first is encoded in mitochondrial DNA, and the other in nuclear DNA. These two sets were associated with a mitochondrial complex basis for oxidative phosphorylation, producing energy in the form of ATP. Interestingly, while the mitochondrial genes themselves were almost not affected, the nuclear genes associated with the OXPHOS mechanism underwent significant modification, depending on the tissues studied. Micrometric analysis data showed a significant reduction in the regulation of nuclear-encoded OXPHOS genes in diseased tissues. The same reaction occurs in a normally aging brain.
The results of a new study show that certain classes of genes associated with mitochondrial manifestations during oxidative phosphorylation are less pronounced in patients with Alzheimer's disease compared with healthy people.
The study also looks at the manifestation of genes in patients whose brains demonstrate an average level of the disease, known as mild cognitive impairment. Here the opposite effect with the corresponding genes is observed - the reaction is expressed more brightly. The authors believe that this observation may indicate some compensation mechanism in the brain that is trying to prevent the disease in its earliest stages. In addition, they believe that the restoration of a specific set of damaged genes associated with mitochondrial function and located in the nucleus of DNA cells is a possible option to stop the disease.
The results obtained are consistent with data from previous work, which states that the accumulation of beta-amyloids in neurons (a hallmark of Alzheimer's disease) is directly involved in mitochondrial dysfunction. “Our work on mitochondria offers a reliable marker that appears at the very beginning of the disease. It correlates more closely with the degree of dementia than the current diagnosis of plaques and tangles, ”Coleman notes.
The exact mechanisms that affect mitochondrial diminution during aging or Alzheimer's disease remain to be seen. Research shows that treatment methods aimed at restoring gene function may open a new way to cure a disease.
Scientific work published in the journal Alzheimer's & Dementia
DOI: 10.1016 / j.jalz.2016.09.003
Source: https://habr.com/ru/post/399017/
All Articles