Japanese scientists raised eggs from mouse skin cells
Japanese scientists were able to transform mouse skin cells into eggs, and then grow healthy offspring from them. This is the first creation of a genital cell outside the body of a mammal. If this process can be repeated for people, perhaps in the future, humanity will be able to solve the problem of infertility.
Katsuhiko Hayashi, a reproductive biologist from Kyushu University in Fukuoka, together with stem cell specialist Mitinori Saito, managed to reprogram stem cells into embryonic cells and primordial germ cells (PGCs). These cells appear when the embryo begins to develop, and later they give rise to sperm and eggs. Previously, researchers had to transfer them into the ovaries of live mice, so that they could finally develop there. But now the need for this has disappeared. The Saito and Hayashi method allows scientists to create an unlimited number of PZK that were previously difficult to obtain. This discovery stimulated research in the field of mammalian reproduction.
')
In mice, germ cells appear in the first week of embryonic development, in an amount of about 40. This small group continues to form the tens of thousands of eggs that female mice have at birth and millions of sperm cells in males.

Over the 10 years of hard work, Saito and his team have identified several genes - Stella, Blimp1 and Prdm14, which in a certain combination play a crucial role in the development of the PZK. Using these genes as markers, they could select the PZK from among other cells and study what was happening to them. In 2009, during experiments at the Center for Developmental Biology at the Institute for Physical-Technical Research ( RIKEN ) in Kobe, it was established that, under all the conditions necessary for cultivation, the addition of bone morphogenetic protein Bmp4 leads to a transformation of PZK. To test this principle, Saito added a high concentration of Bmp4 to fetal cells, and almost all of them turned into PZK. He and other scientists expected the process to be more complex.
Later, Saito was joined by Hayashi, who tried to use epiblast cells - a multicellular embryo with a single-layer structure - Saito's starting point. But instead of using individual cells, as his colleague did, he tried to take a stable cell line that could reproduce the PZK. It did not work. After the failure, Hayashi advanced in another study, which showed that activin A molecules and the main growth factor of fibroblasts can transform previously derived embryonic stem cells into cells, akin to epiblasts. So the idea was to use these two factors to induce embryonic cells to differentiate into epiblasts, and then apply the previous Saito formula to push the resulting cells into a PZK. This approach has been successful. To test whether these cells could develop into viable spermatozoa and eggs, Saito introduced them into the testicles of mice that could not produce sperm naturally, and thus restored their fertility. Then the team inseminated with artificially created sperm normal eggs. The result was healthy offspring.
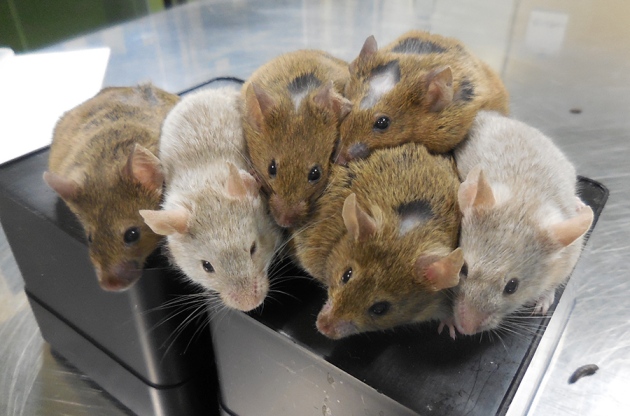
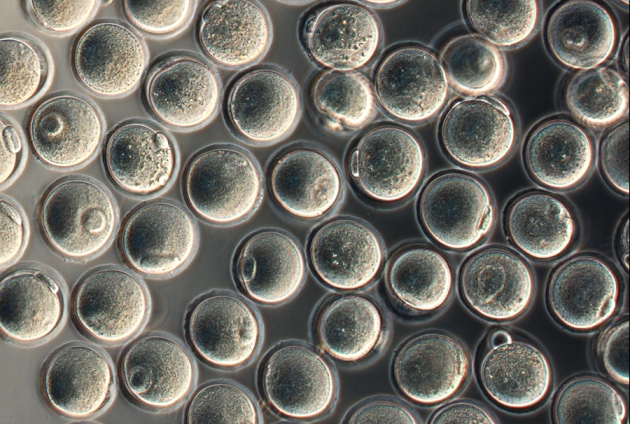
The next major breakthrough in research occurred in 2016, when a team led by Yayoi Obata from Tokyo University of Agriculture reported on the transformation of the PGCs isolated from mouse embryos into oocytes (eggs) without a mammal. Working with Obata, Hayashi and Saito completed the cycle: from the skin cells, they came to functioning eggs in the test tube. When using in vitro fertilization, 26 healthy mice appeared. Some of them were born from the initially available embryonic stem cells, and the other from reprogrammed skin cells. Hayashi says that some of them then gave birth to a second generation of mice. “Parts of this work were done earlier - here they were put together. The fact that they were able to get healthy offspring is impressive, ”notes Dieter Egli, a biologist at the institute of the New York Stem Cell Foundation.
“This is truly amazing,” says Jacob Hannah, a stem cell biologist at the im. Weizmann in Rehovot, Israel. "The ability to reproduce reliable and functional mouse oocytes again and again exclusively in a test tube and observe the process is the most exciting."
Scientists believe that the procedure is reliable, although technically difficult. Hayashi's experiment was repeated by other research teams in his laboratory. Although biologists do not need to implant PZK in live mice, they must add cells taken from the ovaries of the mice to create an ovary in which the egg can be grown. Hayashi is now trying to create an artificial reagent that could replace these cells. The test cell in the test tube is a significant step forward after scientists in China announced in February that they had taken elementary sperm in a test tube. In this case, the researchers created "spermatids" that are not truly mature cells, although they claim that they can be used to create offspring.
Hayashi is confident that the result of the work done will help him study the development of the egg, and now he can fully grow them in test tubes. However, he is not trying to create functioning human eggs in the laboratory. Japanese law prohibits fertilization of human designed germ cells, even for purely research purposes. But the scientist suspects that others will try. “I don’t think it will be much more difficult,” notes Hannah, who himself hopes to create human eggs.
Hannah led the team that reported the first artificial human PZK in 2014, just two years after the publication of Hayashi’s work with mice. For ethical reasons, he did not implant them into the human body in order to try to derive spermatozoa or eggs from them. But the prospects for developing human PZK in vitro look tempting. Hanna's lab is already conducting the experiments described in the new Hayashi article. One of the main problems is obtaining the necessary support for ovarian cells (or testicles for sperm). Currently, the process only works with embryonic cells. But he hopes that the cells of pigs or monkeys can work.
Hayashi believes that before the creation of "oocyte-like" human cells - 10 years. He doubts that they will be of high quality so that they can treat infertility. He believes that it is too early to use artificial oocytes in medicine. ” He also warns that mice artificial eggs are often of poor quality - they can produce embryos with genetic abnormalities or potentially unhealthy offspring. According to the results of the study, only 3.5% of early embryos created from artificial eggs resulted in the appearance of offspring, compared with 60% of eggs that have matured in the womb of the mouse.
Source: https://habr.com/ru/post/372789/
All Articles