Large FAQ about different types of vision correction: all geek questions in one place
Below is a direct comparison of the types of correction (operations) with a convenient summary of possible complications and applicability, plus a sea of other questions from professional paranoids: from “what happens if you give a head during the operation” to “will I give the fabric that I took out of my eyes ”and“ what will happen in old age with my eyesight. ”
- Which is better: glasses, lenses or laser correction?
If you are completely satisfied with the glasses - keep calm, the correction is not necessary. However, if you have never tried lenses, then you should try to wear them for a couple of weeks to understand how the world will look after correction. In the 10-year term, contact lenses (even one-day) are much more dangerous than correction for reversible and irreversible side effects and complications. Therefore, I recommend them only for familiarization with the brave new world.
')
- I decided to stay on the glasses, but I am afraid that the car cushion will open in my face and they will become contact lenses. What to do?
In my surgical experience, modern airbags do not injure eyeglasses. The eyes and face are usually damaged by shards of the windshield. If you are concerned about the safety of glasses, then think about modern, with polycarbonate lenses. They are incredibly durable: the car drives on crash tests.
If you see badly and don’t wear glasses, then you lose some of the information about the world around you and at the same time create additional strain on the visual apparatus. There is a problem - optical correction is needed. And you can ruin your eyes with glasses, as one of our colleagues from a clinic in the city of Marburg - he fell asleep in glasses at a computer at home, fell face down on a keyboard, and a piece of glass entered the lens. My partner, Walter Sekundo, operated on him: they first replaced the lens, then a year later they needed a transplant.
- What else is worth knowing about the glasses?
Intuitively, glasses should be as wide as possible for the peripheral vision to work (at least somehow). Nevertheless, it has not yet been clinically proven that the effect of observation through the center of the lenses (and this is how most of those who wear glasses look) creates some problems for the mechanics of the eye. In general, this can not be afraid.
The choice of lenses for glasses should always begin with a visit to an ophthalmologist. Only a specialist can write a prescription for glasses. Before this, visual acuity is checked to determine which optical characteristics of the lenses (diopters, the distance between the pupils) are appropriate in your case. The choice of the type of lenses - one of the main stages. There are plastic and glass lenses, lenses with anti-reflective coating, darkened, refined, etc. - each type has its own functionality.
For example, chameleon glasses (photochromic) are good for a sunny climate, now they are recommended even to children. In addition, "chameleons" can be used by drivers, as there are eyeglass lenses that darken behind the windshield. In the north, where the glare of snow (for example, climbers to protect against "snow ophthalmia") is traditionally used glasses with a polarizing effect.
- And if contact lenses, which ones are better?
One-day lenses are better than two weeks, and those are better than long-wearing lenses. But they are all rather unsafe in the long term. The main danger of contact lenses (in terms of significant degradation or loss of vision) is bacterial keratitis, that is, inflammation of the cornea. You take the lens conditionally with “dirty” hands, set it in the eye, pour it with almost saline solution - and a kind of Petri dish forms between the lens and the cornea, where bacteria begin to vigorously and actively proliferate. That is why all the instructions to the lenses five or six times written about the need for hygiene and what to do if the eye suddenly became ill, itched, reddened or something else happened.
There is more about lenses here .
- What about perforated glasses?
These are glasses with small holes. Here, the effect of the camera obscura acts; these glasses due to a significant decrease in the aperture of the eye pass only conditionally parallel rays into the eye, which ensures a very large depth of the sharply depicted space. They can sometimes be useful in irregular optical environments, but they are not a “simulator.” Their much more interesting application is the pseudo-accommodation trick. When focusing (accommodation) of the lens does not work in a person, and these are age-related changes in people of presbyopic age or cases of implantation of an artificial lens, it can be achieved by reducing light scattering of a fairly good effect for a number of cases with such glasses.
- What short-sightedness and farsightedness can be corrected and when?
Any degree of myopia can and should be corrected if it interferes with living. Age - from 18 years old to very old age, but I often recommend waiting for 21 years to complete the formation of a corneal stroma. With the help of phakic lenses, myopia can be corrected to -20 diopters in case of ICL implantation (posterior chamber of the eye) and up to -24 diopters in case of working with the anterior chamber of the eye (a bit more risky), this is a more invasive operation.
Hyperopia is usually corrected by a laser to +6 diopters, then lenses and other methods (such as replacing the lens with an artificial one). In general, if you have severe myopia or farsightedness, it is necessary to undergo a diagnosis - much depends on the state of the cornea and its thickness, there is no universal answer.
- What are the types of operations?
The history of correction operations is here .
- Is it possible to give birth after laser correction?
Yes, it is possible without restrictions. Any method of laser vision correction does not affect childbirth. Even the presence of a “cap” after LASIK does not matter. In the USSR, there was a myth about the risks of retinal detachment under loads (weightlifting, childbirth, etc.) after correction - it has already been proven that this is not so. In the US, there was a popular myth that women with high degrees of myopia need to give birth by cesarean section, otherwise there will be vision problems. It is also proven that this is not the case at all. In general, both sports stress and childbirth are normal physiological states. The main limitations are connected with the state of the retina: if there are zones in it that are dangerous in terms of detachment (they need marginal laser coagulation) or there is already retinal detachment, then a cesarean section.
Correction is not done during pregnancy and during lactation. I recommend to wait another couple of months after the end of feeding, so that the hormonal background is fully normalized.
- What about presbyopia and its combination with correction?
One of the most common myths is that with age the “minus” will turn into a “plus” and then points may not be needed. This is not true. Simplifying: in the eye there are two main optically strong lenses - the cornea and lens. A healthy cornea after 18 years of age varies slightly and its optical power can be considered constant. But the lens with its ligamentous apparatus is responsible for focusing close and distant. In his youth, he reacts "quickly and flexibly", and with age begins to change. Its density, configuration, size, and transparency change. Simplifying it again, it becomes less elastic and less transparent. And if problems with its transparency usually come back after 60-70 years, then presbyopia (age-sightedness) begins to appear due to a change in its elasticity after 40 years. Moreover, by the age of 50, all people without exception. Then this effect increases with age, again - all without exception. 100% of people are subject to the process, regardless of whether they have optics of the eye - with short-sightedness, long-sightedness, with or without astigmatism.
This is manifested as:
Thus, presbyopia weakens the accommodation of the eye every year - the ability to focus at different distances. On average, by the age of 60, it is completely lost. Vision correction (any type) allows you to go from points 2-4 to point 1. That is, it does not change the elasticity of the lens (these are two unrelated processes, correction is made on the cornea), but you can be relieved of two pairs of glasses, as healthy, and difficulties will manifest only at close range with a full distance correction.
Should I make a correction at the age of 20, 30, 40 or 50 years? In most cases worth. In this case, the refractive surgeon always takes into account the age of the patient when choosing a correction algorithm and method. Presbyopic patients with transparent lenses older than 45–50 years of age discuss the feasibility of a complete correction of myopia, since residual minor undercorrection on one (not the leading eye) or both eyes would ease the visual load for near. Farsightedness and astigmatism always correct completely, as they interfere with vision and into the distance and near.
- I am very afraid that someone will fit me with a laser, and then with a piece of iron in the eye. Can it be anesthetized?
In theory, it is possible, and sometimes they even do it, but I do not recommend it in standard cases. There is only 20-25 seconds of potential fear, and in fact you will not feel or even see anything. If it turns out that your anxiety is excessive, we will give you a sedative that will reduce emotional stress.
- I'm afraid to pull my head during the operation ...
You will not work. The smart bed quite reliably fixes the head. In the case of an excimer operation, autotracking with a high-speed camera operates in the phase of laser operation, which monitors the position of the eye and drives the laser accordingly. In the case of ReLEx-methods, it is still more reliable: the eye is fixed by pneumocapture, you will not have a desire to move the eye, since anesthesia of the surface of the eye is quite strong. In the event of a pressure drop in the pneumatic pickup below the recommended one, the laser stops and allows the operation to continue from the place of the stop. In the second part of the ReLEx, when it comes to the manual part of the operation (extracting the lenticles), everything is also quite simple: the doctor leans on your forehead, your head is in a special soft grip, plus the eye is additionally held by forceps, second hand. Accidentally make a breakthrough will not work. In addition, an experienced surgeon constantly talks with the patient during the operation - about half of our patients think that there is still a calibration, when everything is over. As an additional convenience, we give you a ball-anti-stress (at the request of the patient, this is sometimes the nurse's hand), this eliminates fine motor skills. Another important point - while the laser is operating, the patient should not talk and move. This gap is only 26 seconds! Regardless of which minus we correct: -1 diopters or -10 diopters. During this time - only 26 seconds - you need to look at the green light, which is located directly in front of the eye. The first 15 seconds the light is clearly visible, the next time it is not clearly visible or disappears completely. This is normal - the resulting layer of gas bubbles in the cornea shields a green light. After 15-20 minutes the gas bubbles almost completely dissolve, and the picture is adjusted.
- I'm paranoid. The laser had to be stopped, I did not get into 99.99% of normal operations. What's next?
In approximately 50% of cases, it will be possible to continue normally, but the surgeon will have to make a small incision at the stopping point with a diamond scalpel (a small uncut bridge is formed there). In some cases (approximately 40%), it will be necessary to make a wide cut, that is, to change the operation from SMILE to FLEX - it is more invasive, but the quality of the correction is the same. This was twice in 8 years in a German clinic, both patients did not experience complications. In about 10% of cases a different type of correction will be required. A micro incision in the eye itself has almost no effect, the key change in mechanics is precisely the extraction of the cut lentikula lens and the collapse of the resulting cavity. In general, in the case of a complex stop, we recommend waiting 2 hours before the gas leaves the cavitation bubbles completely - this is necessary not only for the surgeon to make an informed decision and make diagnostics again, not on the fly, but also for the patient to calm down .
- And if the laser firmware “fails” or the processor breaks - will my head be cut off?
The laser has other tasks. "ATM" Windows provides only the interface, the key things are done with specialized software. Errors are mechanically monitored — for example, a pneumatic pickup manometer immediately breaks the circuit and shuts off the laser in the event of a capture pressure decrease. At this point, the laser stops “automatically”, and the software records the coordinates of the stops to return and continue. Modern lasers are able to find a stop and continue the operation. In the event of a power failure in the operating room, the built-in laser batteries are triggered, even the standard medical UPS of the operating unit is not needed for this, there is enough time for the whole operation. The excimer laser additionally requires calibration at the beginning of each trading day — cuts out a dozen calibration lenses on a special polymer pad. Before the operation on each eye, the laser system performs additional self-diagnostics, in case of deviation of at least one of the parameters, the surgeon cannot start the procedure. Nevertheless, the surgeon has two ways to control the laser: pressing the pedal (remove the leg - turn off the laser) and, additionally, there is an emergency stop button on the front panel of the laser housing.
- What about licenses?
For the past few years, major laser manufacturers have required a separate license for each operation. Replaceable disposable parts (cones adjacent to the eye) are supplied with a license package. On some lasers, these are hardware keys (cards), on others, a combination of letters and numbers that need to be driven into the interface in advance. For each type of operation and each individual eye - a separate license.
One of the most complicated licensing procedures is provided by VisuMax - first of all, the equipment manufacturer Carl Zeiss licenses the doctor, he must undergo training on pig eyes (WETLAB), then he must do 50 eyes with FLAP technology, 50 eyes with FLEX technology and only after that he gets permission to use technology ReLEx SMILE.
By the way, if you are planning a SMILE operation, you can always ask Zeiss if the surgeon has a license for this.
The clinic may not receive a number of licenses. For example, first a new doctor needs to do a dozen training operations on pig eyes, then you can get licenses for FemtoLASIK, after gaining experience - on FLEX, and already after about 70 operations in total - on ReLEx SMILE. Immediately do complex operations, no one will.
- How to reduce the risk of complications?
Here are the main dependencies:
Here are more details , and here - the consequences of complications and diagnosis.
Thus, with a good diagnosis, even a novice surgeon can perform the operation without difficulty. But if something goes wrong (a chance of 0.5%, I remind you that these are statistics of experienced surgeons), it is better that there is an opportunity to make a further decision together with an experienced colleague. That is why novice specialists do the first 50-100 operations (after training in the pig's eyes) themselves, but an assistant with extensive surgical experience is close by.
Technologically, there are special methods that allow additional correction after laser correction, carried out by any of the existing methods for today - for SMILE, FemtoLASIK, LASIK or PRK. How exactly - decide the doctor.At the European Congress ESCRS in Copenhagen last year, one of the leading refractive surgeons in the world practicing in London, Dan Renstein, gave a report that listed 5 different methods of correction in various cases. So, if the patient suddenly needs, there is plenty to choose from. After SMILE, the quality of optics on 6th generation lasers is consistently higher than after LASIK or FemtoLASIK, the probability of optical side effects is significantly less. When we are planning a laser correction, we expect that this procedure is done only once in a lifetime. The percentage of the correction on the generalized international statistics for SMILE is the lowest today - about 0.5%. In specialized clinics with experienced doctors, it is significantly less. I repeat, specifically, we did not have them, but the probability cannot be ruled out, and therefore - so far, ratherquestion of experience and luck.
- How will the operation go?
Consider the example of ReLEx SMILE.
Here there are details about how the laser works - if very briefly, it creates a focusing point in the thickness of the cornea, a microexplosion occurs there, then a cavitation bubble forms and the plasma gently pushes the tissue around the focus point. A chain of such pulses forms a res.
Here is more detailed about the course of the operation and what you will see. About related questions - here .
The operation on both eyes takes 10-15 minutes.
- What you need to know about the cornea?
The cornea is the most complex formation that is formed in embryogenesis from three different types of tissue: surface ectoderm (epithelium develops), mesoderm (stroma) and neuroectoderm (endothelium is formed). As it develops (differentiated), each of these tissues needs the isolation provided by boundary shells to preserve its structure and specificity. Thus, the endothelium forms the Descemets sheath, and the stroma - the Bowman's sheath. Here is the diagram:

1. corneal epithelium; 2. Bowman's membrane; 3. corneal stroma; 4. Descemetov shell; 5. corneal endothelium.
The corneal epithelium is a multilayered tissue, cells in 5-7 rows. It protects the eye mechanically, does not let microorganisms and small mote, provides an immune response. Mucin of the tear film fills all the irregular elements in the surface epithelium, which provides a smooth transparent surface. Like the normal epithelium of the skin, it regenerates well, and during PRK surgery it is removed to gain access deeper. Within a few days, it is restored.
The second layer is the Bowman's membrane. This is a thin layer immediately below the epithelium. Does not contain cells, consists of randomly arranged collagen fibrils. Some animals do without it in principle. In humans, at least performs the function of compensation of intraocular pressure and a number of other tasks that are not yet fully understood. The Bowman's membrane cannot be restored after damage, therefore, after corneal damage in this part, scars are formed at the site of defects and the transparency of the cornea in these areas is disturbed and turbidity is formed. When laser correction lenses are formed deeper. However, at any cut through the bowman's membrane, we cut the nerves, of which there are quite a few. In PRK, the membrane is removed entirely to gain access to the stroma. Just in the Bowman's membrane, which, due to congenital or acquired inferiority, ceases to perform the barrier function, keratectasia begins.
With minimally invasive removal of lenticules with ReLEx, there is only one short cut (2.5 mm), and not nearly the entire circumference, as in the case of LASIK / FLEX-like methods. It is damage to the Bowman's membrane that disrupts the epithelization of the eye, innervation, and other side effects.
The next part of the cornea is the stroma. This is where the main work goes. Fabric - collagen filaments impregnated with hyaluronic acid. When magnified, they resemble ropes. These parallel plates are formed from collagen fibrils. They know how to merge. If the ropes stick one into the other, then with the formation of nodes-adhesions, and this prevents visual acuity.
But, being laid on each other overlap (that is, from different angles), they do not form these knots, but simply interlock. During the laser correction ReLEx SMILE we cut the lens in this layer and remove it. After the operation, the cavity in the cornea closes in - the “ropes” lie on top of each other, but at the sites of the incisions a clear boundary does not form from the joints, that is, everything remains transparent (splices of single collagen filaments occur at the border of the lens, that is, in outer diameter). The skeleton is supported as usual - with the Bowman membrane stretched from above and the lower layers.
The next two layers — the Descemets membrane and the endothelium — have little interest in laser correction, since we are not affected by these operations. This is actually a soft and hard boundaries of the body, a kind of standard "casing" for the body.
- “Glass Worms”, which are DST, what about them?
With them is a completely different story . In short - in most cases you don’t have to touch them, the risks of complications, laser shooting of the vitreous body are still there. But if they are very dense and interfere (for example, one of the truckers complained about a “blizzard in the eyes when braking”) - you can correct it. Only a specialist can decide whether to work with a laser or have an operation. Surgery - vitrectomy (removal of the vitreous body). It is quite serious in depth of penetration - as the retina is located near, it refers to high-tech types of operations.
The risk to benefit ratio is always strictly evaluated.
- What you need to know about the price?
Prices for laser vision correction may vary significantly. First of all, first of all, the cost depends on the chosen correction method, since this, in turn, is determined by the cost of the license of the manufacturer (the license for SMILE or IRC is much more expensive than FLEP). All modern lasers have licenses to perform a certain type of correction - for example, personalized LASIK is sold under separate more expensive licenses than the standard LASIK.
The old antediluvian lasers (excimer and femtolasers of the old generation) did not have a license, but performed a poor quality correction. Until now, many clinics work for them - these are just options for “Buy a coupon” or “Discount - 50%”, because these obsolete machines have paid for themselves for a long time, but the equipment is not updated.
Secondly, of course, there is a dependence on the region, on the country, etc. For example, in our SMILE EYES Augenklinik Moskau department, the cost of correcting the vision using the SMILE method agreed in the holding is cheaper than in Germany and Austria. We have 105,000 rubles for the cost of one eye - at a price of 2,500 euros (175,000 rubles) in European offices.
By the way, Professor Sekundo from Germany operates in Moscow at the European price, but his patients save on travel and accommodation when choosing the Moscow branch. And, for example, in the UK the leading refractive above the mentioned surgeon costs three times as much. But in any case, this high-tech micro-invasive method all over the world is quite expensive and is not covered by insurance. If it is offered cheaply, it is probably for the surgeon or for the clinic the starting point. Or the results of mass surgery are not good - SMILE, like no other technique, is individual.
Thirdly, there is a dependence on the obligations that the clinic assumes. For example, the standard in SMILE EYES in all branches, including our Moscow branch, is a guarantee for observation during the year and potential correction, which is possible in the unlikely case.
Fourthly, there are such clinics where such cost as “presence of astigmatism”, “thin cornea”, “difference between the eyes”, etc., influence and additionally pay for the cost. As a result, the initially declared cost increases significantly. In my opinion, this is wrong. The SMILE procedure takes 26 seconds, regardless of minus and astigmatism, the thickness of the cornea also does not affect, even strabismus does not affect! In these cases, either the surgeon does not understand what he is doing, or this is a commercial trick.
Fifth, the cost is influenced by which surgeon performs the operation. In our clinic, these operations are performed by professors, young doctors do not make this type of correction. Let me remind you that the company Zeiss certifies each surgeon (and often it happens that a license is for one, and performs another under his last name - it makes sense to check before choosing a surgeon). In some clinics there is a surcharge for surgery by a professor, “just a doctor or cms” is cheaper - this depends on the policy of the clinic.
In any case, I believe that laser vision correction is a great investment in your health and quality of life.
- In the end, how best to prepare for the correction?
If you have decided that you need correction, then you need to start with a comprehensive diagnostic examination in order to understand whether you have any contraindications and which method will be best for you.
It is important that the clinic where you are applying has the full range of technologies: the possibility of SMILE, FemtoLASIK, sometimes just LASIK or even PRK is needed. Because if there is no clinic, for example, a VisuMax laser and a doctor who can work on it, then SMILE, alas, will not offer you, but will only recommend what is available and tell you what is best for you.
If there is no femtolaser, they will say that LASIK (for example, super-LASIK or epi-LASIK is the pinnacle of evolution!). Unfortunately, not a single clinic, even with a “killed” laser and “killed” diagnostics, writes that it has “old equipment” - you have to either trust or check.
By the way, data from other clinics can be used for preliminary consultation on the choice of technology and the possibility of correction (if they are in full).
The clinic, which will carry out the correction, is obliged to conduct a full examination on your own - in such a case as surgery, you can not rely on other people's research, everything must be rechecked.
So, first of all, it is necessary to undergo a comprehensive diagnosis in the clinic, in which there is the maximum of all modern correction technologies. If you are using contact lenses, it is advisable to switch to glasses for 1-2 weeks before the diagnosis.
Diagnostics in time is usually not a quick process, takes 1.5-2 hours and after that options of technologies that suit you are offered. In the case of SMILE, the "cherished" global 0.5% of complications on the 6th generation can be reduced to 0.1-0.2% simply due to a comprehensive diagnosis.
Pre-domiciliary, you can take the necessary set of tests recommended by the Ministry of Health of the Russian Federation (we give out the list) or you can do this in our clinic.
You need to come to the surgery without makeup and smelling perfume. Alcohol is better to exclude from the dinner menu the day before.
You need to take your passport and sunglasses with you; you will receive all the accessories you need for the operation in the clinic.
On the day of surgery, special preparation is not necessary, as a rule, you spend a couple of hours in the medical center and then go home yourself. Maintenance is not necessary, the eyes will see quite well (on average, 3-5 lines on the table) within an hour after the operation.
But we prohibit independently driving, you can only drive a car the next day after the operation. It is better not to plan anything serious on the day of the operation, to rest and put off important matters.
The next day you can walk, ride a bike, engage in active sports, usually wash. Immediately after surgery for a couple of hours, you may experience discomfort (from light cramps to moderate tearing) - this is a normal reaction of the body to damage to eye tissue. These symptoms are strongly pronounced after FemtoLASIK or LASIK and an order of magnitude less after SMILE.
After PRK, the pain will persist for two weeks - this is not the most pleasant operation. The next day after surgery, you are monitored by a doctor, then after a week or two. The next inspection is in 3 months, then in 10-12 months.
If you have any unplanned questions - you can always make an appointment and come for a visit to dispel your doubts. You can write by e-mail - your doctor will answer you. But we must remember that, not seeing you, the doctor can not make a diagnosis by phone or change the treatment regimen.
Operations on two eyes are done on the same day. In theory, of course, you can spread for several days, but it is inconvenient and has no medical indications.
Another point - after correction, people in many professions (for example, chemists, cooks, etc.) need to be careful if they have worn glasses before. During the years of wearing glasses over their eyes, they have the feeling that you can bend your head directly over the pan or not wear special protection in the laboratory. After the correction, it takes several weeks to get used to the fact that the oil from the frying pan is splashing, and protection is needed in the chemical laboratory.
- How does the correction for boys differ from the correction for girls?
Nothing. The eyes of men and women are the same, the risks too. Let me remind you once again that pregnancy and the feeding period for girls is a time when the correction cannot be done. I recommend to return to the question of correction 6-8 months after the end of lactation.
By the way, for medical reasons, laser correction can be done at an earlier age.
The recommended age for correction is from 18 years and older, but there is no age limit in a big way. But all, of course, individually.
- What correction do?
The doctor will tell. SMILE is an advanced technology that has enriched the repertoire of laser-refractive surgery to make them even safer and more comfortable. The question should not be that it is good, but that is bad, but that an individual approach is needed. And each method has its pros and cons. If the patient is young, and even the cornea is thinner, then undoubtedly, the best technique is SMILE, because there is less risk of keratectasis, more stability of the achieved effect and excellent vision the next day with phenomenal comfort. The same for a person at the age of 50 is easier to treat with FemtoLASIK (it does not mean that it is better): the cornea is harder (less risk of keratectasia), and the next day it will probably see better than after SMILE, because a hard cornea needs more time adaptation of the internal slice. A dry eye, of course, will torment longer, but after six months the difference is gone. Well, if you need an economical option, then PRK will also give an acceptable result with a little myopia. Therefore, FemtoLASIK, SMILE and even PRK (especially for refractions in the region of 1 diopter) are able to exist next to each other.
Ordinary LASIK, this excellent operation by the standards of two thousandths, today needs to be done in exceptional cases (for example, scars in the cornea). Despite the persuasion and all advertising words - the other options are better. In your particular case, most likely, the relief features of the cornea’s surfaces and its thickness, profession and hobby, age and much more will fall on this picture - advice is useless without diagnosis.
- What does an IT specialist need to know about vision?
Let's start with platitudes: the less you sit at a computer, the better. The more often you relax and look away, the better. If you are fond of sports such as table or tennis, or badminton, or golf, etc. (where there is a frequent change of focus) is good. Of the average importance of things - watch the light, it is best to use indirect light (for example, a lamp with a lamp shade) so that it is dim and not quite dark. Do not put the monitor so that there is a glare, use matte screens, if you can. There is almost no difference in reading from a tablet or an e-book (there is no research, I can’t justify with numbers), but subjectively - from a well-lit screen, e-ink is better.
The most important thing: if you have a screen at your workplace or at home 13-17 inches, then you can improve your life if you buy a larger display and place it a little further away than the current one - at least 10 cm. And better by 20. Not move the monitor closer to you when reading small text, and increase the font size if you can transfer it comfortably for reading speed.
Rest, take short breaks, leaving the computer: at lunch, go for a walk, and do not sit at the computer, do not be lazy to go to the printer or have a cup of coffee.
There are no clinical data on different types of screens and their flickering, problems were only with screens based on cathode-ray tubes. So, if you work at a computer, and especially from a laptop, it is better to do it at the table, sitting straight and level (this ensures that there are no problems in the cervical spine, that is, as a result, a normal blood supply to the head), often get up and watch out the window.
Long-term work at the computer leads to a violation of the stability of the tear film and to the appearance of such a disorder as “dry eye syndrome”. It is necessary to blink more often or use special moisturizing drops, or put a humidifier.
In general, the eyes of an IT specialist are exactly the same as other people. For an adult, the danger of working at a computer is greatly exaggerated. There is no particular difference between what you would read 8-10 hours a day in the eighteenth century or sit at a computer today.
But, let me remind you, in the eighteenth century, general surgeons provided eye health, there were no antibiotics, ophthalmology was only in its infancy. You are definitely lucky with the twenty first century. But most importantly, you can be calm about the need to change jobs. If you follow the rules - everything will be fine.
Everything!
Seems to be able to answer all your questions in one place. If there is more - ask, I will update the FAQ.
More of our posts, where everything is more detailed:
- Which is better: glasses, lenses or laser correction?
If you are completely satisfied with the glasses - keep calm, the correction is not necessary. However, if you have never tried lenses, then you should try to wear them for a couple of weeks to understand how the world will look after correction. In the 10-year term, contact lenses (even one-day) are much more dangerous than correction for reversible and irreversible side effects and complications. Therefore, I recommend them only for familiarization with the brave new world.
')
- I decided to stay on the glasses, but I am afraid that the car cushion will open in my face and they will become contact lenses. What to do?
In my surgical experience, modern airbags do not injure eyeglasses. The eyes and face are usually damaged by shards of the windshield. If you are concerned about the safety of glasses, then think about modern, with polycarbonate lenses. They are incredibly durable: the car drives on crash tests.
If you see badly and don’t wear glasses, then you lose some of the information about the world around you and at the same time create additional strain on the visual apparatus. There is a problem - optical correction is needed. And you can ruin your eyes with glasses, as one of our colleagues from a clinic in the city of Marburg - he fell asleep in glasses at a computer at home, fell face down on a keyboard, and a piece of glass entered the lens. My partner, Walter Sekundo, operated on him: they first replaced the lens, then a year later they needed a transplant.
- What else is worth knowing about the glasses?
Intuitively, glasses should be as wide as possible for the peripheral vision to work (at least somehow). Nevertheless, it has not yet been clinically proven that the effect of observation through the center of the lenses (and this is how most of those who wear glasses look) creates some problems for the mechanics of the eye. In general, this can not be afraid.
The choice of lenses for glasses should always begin with a visit to an ophthalmologist. Only a specialist can write a prescription for glasses. Before this, visual acuity is checked to determine which optical characteristics of the lenses (diopters, the distance between the pupils) are appropriate in your case. The choice of the type of lenses - one of the main stages. There are plastic and glass lenses, lenses with anti-reflective coating, darkened, refined, etc. - each type has its own functionality.
For example, chameleon glasses (photochromic) are good for a sunny climate, now they are recommended even to children. In addition, "chameleons" can be used by drivers, as there are eyeglass lenses that darken behind the windshield. In the north, where the glare of snow (for example, climbers to protect against "snow ophthalmia") is traditionally used glasses with a polarizing effect.
- And if contact lenses, which ones are better?
One-day lenses are better than two weeks, and those are better than long-wearing lenses. But they are all rather unsafe in the long term. The main danger of contact lenses (in terms of significant degradation or loss of vision) is bacterial keratitis, that is, inflammation of the cornea. You take the lens conditionally with “dirty” hands, set it in the eye, pour it with almost saline solution - and a kind of Petri dish forms between the lens and the cornea, where bacteria begin to vigorously and actively proliferate. That is why all the instructions to the lenses five or six times written about the need for hygiene and what to do if the eye suddenly became ill, itched, reddened or something else happened.
There is more about lenses here .
- What about perforated glasses?
These are glasses with small holes. Here, the effect of the camera obscura acts; these glasses due to a significant decrease in the aperture of the eye pass only conditionally parallel rays into the eye, which ensures a very large depth of the sharply depicted space. They can sometimes be useful in irregular optical environments, but they are not a “simulator.” Their much more interesting application is the pseudo-accommodation trick. When focusing (accommodation) of the lens does not work in a person, and these are age-related changes in people of presbyopic age or cases of implantation of an artificial lens, it can be achieved by reducing light scattering of a fairly good effect for a number of cases with such glasses.
- What short-sightedness and farsightedness can be corrected and when?
Any degree of myopia can and should be corrected if it interferes with living. Age - from 18 years old to very old age, but I often recommend waiting for 21 years to complete the formation of a corneal stroma. With the help of phakic lenses, myopia can be corrected to -20 diopters in case of ICL implantation (posterior chamber of the eye) and up to -24 diopters in case of working with the anterior chamber of the eye (a bit more risky), this is a more invasive operation.
Hyperopia is usually corrected by a laser to +6 diopters, then lenses and other methods (such as replacing the lens with an artificial one). In general, if you have severe myopia or farsightedness, it is necessary to undergo a diagnosis - much depends on the state of the cornea and its thickness, there is no universal answer.
- What are the types of operations?
- Old techniques of technique "by hand". Radial keratotomy - applying incisions from the center of the cornea to the edges (good old Russian-Japanese method, quite invasive, with a lot of complications, but in those years there was no better and it really worked). Then keratomillosis - the invention of Barraquer, who cut off the upper part of the cornea to the patient, froze it, drove to the other end of the city to the jewelry machine, polished and sewed it back to the patient. The accuracy is so-so, but the method, again, worked. Now these methods, of course, are not used, but the experience of doctors with steel scalpels is at the heart of modern ones.
- Photorefractive keratectomy of PRK (and its varieties - transFRK, epilASIK, LASEK, etc.). The oldest laser surgery is when a lens is evaporated over the stroma surface with an excimer laser. Preliminarily, the epithelium layer is removed by some method (mechanically manually, by a keratome, or by the same excimer laser). Unlike other methods, the second layer of the cornea is completely destroyed - the Bowman's membrane, which compensates for intraocular pressure and in which there are quite a lot of nerves. The most studied in clinical practice for today is surgery and simple technically. Even a novice surgeon is hard to spoil it. Among the shortcomings: painful, long recovery (two weeks of tears and burning until the epithelium grows under the contact lens), a high risk of healing with a “hay” (fog in the correction zone). Of the advantages: the exact result on small corrections (less than -2) and you can engage in active sports, because it is a technology without the formation of a “valve”.
In short, after it you will be taken to the German police or American special forces, if the healing was successful. Cheap, does not require highly skilled surgeon, is done almost completely in automatic mode. It is used for weak cornea after crosslinking (enhanced by vitamin B2 with UV treatment to release oxygen and increase collagen strength) as a possible correction method. In Germany, it is done in about 8-10% of cases according to indications and long-standing reputation, plus on minor corrections. More PRK is sometimes used as an additional correction if other methods are not suitable. In the comments they mentioned the PRK with tracking (auto-tracking) - in Estonia they advertised it as a new modern operation, although the technology is already 30 years old.
About varieties of PRK: by any method, scrape the epithelium, cut off, it becomes unviable and under the contact lens you have to wait for the growth of your own in several layers. The greater the minus or plus the PRK has been adjusted, the higher the risk of heyaz. - "Ordinary" LASIK (laser-treated keratomoluses). Using the blade, the top layer of the cornea is cut off, then it is lifted up like a basket lid, then a lens is evaporated under the “lid” using an excimer laser, then the cap is put in place. This is the most common technology in the world - including due to the availability of old models of lasers operating under a “simplified” program, and not requiring great manual skills from a doctor, often available even in small cities. To perform it, in addition to the excimer laser, you need another device - a microkeratome, with which the "cap" is formed. In the modern world, it is increasingly being replaced by femtosecond LASIK. In this case, the same “lid” is formed using another laser - femtosecond, which improves the accuracy of cutting and increases the strength of the connection between the “lid” and the bed in the cornea. It may be the only possible method for corneal scarring (including after keratotomy) - the blade cuts through everything, including coarse scar tissue. Femtolaser is not capable of this.
Modern excimer lasers are distinguished by high accuracy of correction (in comparison with other methods), but also by a 6% chance of complications (this is quite a lot). The main complications are associated with the presence of a "cap", which never grows and is held only by the epithelium. I would absolutely not recommend LASIK in the presence of alternatives, albeit more expensive. There will be restrictions on active sport, a high probability of “dry eye syndrome”, and most importantly, a decrease in the biomechanical properties of the cornea. In Germany (this is the data of the German colleagues of the SMILE EYES holding), the last two years have hardly been done. - FemtoLASIK. The same LASIK, only instead of a steel blade, a femtosecond laser is used to cut the "lid" of the eye, which provides greater accuracy. The most accurate femtolasers for refraction are the 6th generation VisuMax Carl Zeiss. They are also the most comfortable for the patient and the operating surgeon. But FemtoLASIK also has potential problems associated with the presence of a “lid”. The cumulative risk of complications is 2%. The flap “cover” never grows and can be folded as a result of injury (it rests, in fact, on the surface epithelium and thin spike-leg), therefore it is not recommended for people who have the risk of injuring an eye as a result of an active lifestyle or professional activities. But tearing off the “lid” with FemtoLASIK is more difficult than with the usual LASIK.
The operation does not require high manual skills of the surgeon. The Bowman's membrane is badly damaged, almost all nerves are stopped by a laser - this is the main drawback of the method. FemtoLASIK was made in Germany often several years ago, now it is fading away. A few days later you can sit at the computer, play sports. You can go to the pool or bath in a couple of weeks. FemtoLASIK is more expensive than LASIK, since it requires two laser systems - an excimer laser and a femtolaser. - SuperLASIK and approximate analogues. Topoguided operations are done on an individual cornea map for the patient. The “cap” can be formed by both microkeratome and femtolaser. We are talking about the type of profile that models the cornea under you. When laser correction in an individual profile, surgical aberrations are minimized, high-order aberration values are taken into account (they affect the quality of vision, reduce the possibility of side optical effects). SuperLASIK using a license for an individual profile is more expensive than a standard LASIK.
- FLEX. Intermediate evolutionary stage. The same FemtoLASIK, but with an important difference - instead of an excimer laser, a femtosecond lens is used to evaporate a lens for ultra-precise cutting. Simple geometry (one almost even section) provides significantly less invasiveness, less energy comes into the eye. The method is demanding of the surgeon’s manual skills and injures the Bowmen membrane, does not allow to engage in active sports. These operations today are done in 90% of cases, as a replacement for FemtoLASIK according to the surgeon training protocol for SMILE (FLEX experience is needed), so you have a chance to get them very cheap or almost free of charge when training a surgeon.
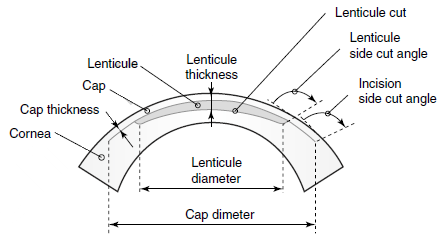
- ReLEx SMILE (SMall Incision Lenticula Extraction - minimally invasive lenticular extraction). This is a method where a kind of counterform for a lens (lenticle) is cut inside the corneal stroma, then it is removed through a thin “tunnel”, the stroma collapses and settles, and a new shape of the cornea is formed. To remove lenticles, the eye does not open, and the “cap” does not exist: the femtosecond laser models the “lens” in 3D format right inside the cornea without damaging its surface. Then a small tunnel is cut into the lens of a complex shape (incision 2.0-2.5 mm wide in the cornea), through which this lens is taken with forceps.
The most minimally invasive method, preserves the Bowman membrane and 90% of the nerves in it (only those that the incision passes to extract lenticules are damaged). On the 6th generation lasers, the correction accuracy is higher or equal to FemtoLASIK - from -1 to -10 diopters. On lasers of the 5th generation - 4% lower. You can also make correction to patients with myopic astigmatism or myopia with astigmatism. Allows you to freely engage in active sports. For the computer, on fitness or in a trip it is possible the next day.
A generalized indicator of reversible and irreversible complications - from 0.5 to 1% (collected on the 5th generation of lasers, on the 6th below). Demanding on the surgeon’s manual skills and experience. Significantly more expensive than FemtoLASIK. In Germany, it is done in about 85% of cases, gradually replacing FemtoLASIK.
On the left - the usual location of the nerves. In the center - after the LASIK or FLEX procedure (where a flap cutout is required). Right - after the procedure ReLEx SMILE. The dotted line shows the borders of the lenticules, the solid line shows the incision through which it is removed from the eye. - Implantation of phakic IOL (intraocular lenses). This is an introduction to the eye of additional correction lenses while maintaining your own lens. The method is good because it allows you to make a correction up to -30 diopters, which the laser does not take, plus it has a number of possibilities for situations where laser correction is impossible due to contraindications. This method is more expensive than laser correction. Phakic lenses are calculated individually and often an individual order must be waited for one to two months. After surgery, after a couple of weeks, you can return to normal lifestyle and sports. This operation belongs to the class of abdominal, so I strongly do not recommend doing both eyes at once in one day. Another point: in Europe, the limit on the IOL is 24 diopters, there is less available line of lenses.
- Remove your own lens and replace it with an artificial (IOL). The human lens is a strong lens, so when replacing it, you can calculate the diopter so as to at the same time correct the shortcomings of optics. In certain cases, this operation is used precisely for correction (in the presence of high ametropia). Correction is an additional opportunity that should be used during the replacement of the lens. In this way, extremely high degrees of myopia, hyperopia, high astigmatism, and presbyopia can be corrected. This operation, unlike the others, is covered by insurance if it is a cataract.
The history of correction operations is here .
- Is it possible to give birth after laser correction?
Yes, it is possible without restrictions. Any method of laser vision correction does not affect childbirth. Even the presence of a “cap” after LASIK does not matter. In the USSR, there was a myth about the risks of retinal detachment under loads (weightlifting, childbirth, etc.) after correction - it has already been proven that this is not so. In the US, there was a popular myth that women with high degrees of myopia need to give birth by cesarean section, otherwise there will be vision problems. It is also proven that this is not the case at all. In general, both sports stress and childbirth are normal physiological states. The main limitations are connected with the state of the retina: if there are zones in it that are dangerous in terms of detachment (they need marginal laser coagulation) or there is already retinal detachment, then a cesarean section.
Correction is not done during pregnancy and during lactation. I recommend to wait another couple of months after the end of feeding, so that the hormonal background is fully normalized.
- What about presbyopia and its combination with correction?
One of the most common myths is that with age the “minus” will turn into a “plus” and then points may not be needed. This is not true. Simplifying: in the eye there are two main optically strong lenses - the cornea and lens. A healthy cornea after 18 years of age varies slightly and its optical power can be considered constant. But the lens with its ligamentous apparatus is responsible for focusing close and distant. In his youth, he reacts "quickly and flexibly", and with age begins to change. Its density, configuration, size, and transparency change. Simplifying it again, it becomes less elastic and less transparent. And if problems with its transparency usually come back after 60-70 years, then presbyopia (age-sightedness) begins to appear due to a change in its elasticity after 40 years. Moreover, by the age of 50, all people without exception. Then this effect increases with age, again - all without exception. 100% of people are subject to the process, regardless of whether they have optics of the eye - with short-sightedness, long-sightedness, with or without astigmatism.
This is manifested as:
- A person with a beautiful vision starts reading with glasses: the lens is hard to “shrink” so that the eye can focus close.
- Myopic ceases to see more and close. As a result, being in glasses for distance and for reading, he will be forced to wear a second pair of glasses or read, removing glasses for distance and bringing the text to his eyes.
- Far-sighted starts to wear 2 or even 3 pairs of glasses: for distance, for medium distance (for example, for a computer) and the strongest points for close range.
- He who also has astigmatism, sees not clearly at all distances and also requires several pairs of glasses.
Thus, presbyopia weakens the accommodation of the eye every year - the ability to focus at different distances. On average, by the age of 60, it is completely lost. Vision correction (any type) allows you to go from points 2-4 to point 1. That is, it does not change the elasticity of the lens (these are two unrelated processes, correction is made on the cornea), but you can be relieved of two pairs of glasses, as healthy, and difficulties will manifest only at close range with a full distance correction.
Should I make a correction at the age of 20, 30, 40 or 50 years? In most cases worth. In this case, the refractive surgeon always takes into account the age of the patient when choosing a correction algorithm and method. Presbyopic patients with transparent lenses older than 45–50 years of age discuss the feasibility of a complete correction of myopia, since residual minor undercorrection on one (not the leading eye) or both eyes would ease the visual load for near. Farsightedness and astigmatism always correct completely, as they interfere with vision and into the distance and near.
- I am very afraid that someone will fit me with a laser, and then with a piece of iron in the eye. Can it be anesthetized?
In theory, it is possible, and sometimes they even do it, but I do not recommend it in standard cases. There is only 20-25 seconds of potential fear, and in fact you will not feel or even see anything. If it turns out that your anxiety is excessive, we will give you a sedative that will reduce emotional stress.
- I'm afraid to pull my head during the operation ...
You will not work. The smart bed quite reliably fixes the head. In the case of an excimer operation, autotracking with a high-speed camera operates in the phase of laser operation, which monitors the position of the eye and drives the laser accordingly. In the case of ReLEx-methods, it is still more reliable: the eye is fixed by pneumocapture, you will not have a desire to move the eye, since anesthesia of the surface of the eye is quite strong. In the event of a pressure drop in the pneumatic pickup below the recommended one, the laser stops and allows the operation to continue from the place of the stop. In the second part of the ReLEx, when it comes to the manual part of the operation (extracting the lenticles), everything is also quite simple: the doctor leans on your forehead, your head is in a special soft grip, plus the eye is additionally held by forceps, second hand. Accidentally make a breakthrough will not work. In addition, an experienced surgeon constantly talks with the patient during the operation - about half of our patients think that there is still a calibration, when everything is over. As an additional convenience, we give you a ball-anti-stress (at the request of the patient, this is sometimes the nurse's hand), this eliminates fine motor skills. Another important point - while the laser is operating, the patient should not talk and move. This gap is only 26 seconds! Regardless of which minus we correct: -1 diopters or -10 diopters. During this time - only 26 seconds - you need to look at the green light, which is located directly in front of the eye. The first 15 seconds the light is clearly visible, the next time it is not clearly visible or disappears completely. This is normal - the resulting layer of gas bubbles in the cornea shields a green light. After 15-20 minutes the gas bubbles almost completely dissolve, and the picture is adjusted.
- I'm paranoid. The laser had to be stopped, I did not get into 99.99% of normal operations. What's next?
In approximately 50% of cases, it will be possible to continue normally, but the surgeon will have to make a small incision at the stopping point with a diamond scalpel (a small uncut bridge is formed there). In some cases (approximately 40%), it will be necessary to make a wide cut, that is, to change the operation from SMILE to FLEX - it is more invasive, but the quality of the correction is the same. This was twice in 8 years in a German clinic, both patients did not experience complications. In about 10% of cases a different type of correction will be required. A micro incision in the eye itself has almost no effect, the key change in mechanics is precisely the extraction of the cut lentikula lens and the collapse of the resulting cavity. In general, in the case of a complex stop, we recommend waiting 2 hours before the gas leaves the cavitation bubbles completely - this is necessary not only for the surgeon to make an informed decision and make diagnostics again, not on the fly, but also for the patient to calm down .
- And if the laser firmware “fails” or the processor breaks - will my head be cut off?
The laser has other tasks. "ATM" Windows provides only the interface, the key things are done with specialized software. Errors are mechanically monitored — for example, a pneumatic pickup manometer immediately breaks the circuit and shuts off the laser in the event of a capture pressure decrease. At this point, the laser stops “automatically”, and the software records the coordinates of the stops to return and continue. Modern lasers are able to find a stop and continue the operation. In the event of a power failure in the operating room, the built-in laser batteries are triggered, even the standard medical UPS of the operating unit is not needed for this, there is enough time for the whole operation. The excimer laser additionally requires calibration at the beginning of each trading day — cuts out a dozen calibration lenses on a special polymer pad. Before the operation on each eye, the laser system performs additional self-diagnostics, in case of deviation of at least one of the parameters, the surgeon cannot start the procedure. Nevertheless, the surgeon has two ways to control the laser: pressing the pedal (remove the leg - turn off the laser) and, additionally, there is an emergency stop button on the front panel of the laser housing.
- What about licenses?
For the past few years, major laser manufacturers have required a separate license for each operation. Replaceable disposable parts (cones adjacent to the eye) are supplied with a license package. On some lasers, these are hardware keys (cards), on others, a combination of letters and numbers that need to be driven into the interface in advance. For each type of operation and each individual eye - a separate license.
One of the most complicated licensing procedures is provided by VisuMax - first of all, the equipment manufacturer Carl Zeiss licenses the doctor, he must undergo training on pig eyes (WETLAB), then he must do 50 eyes with FLAP technology, 50 eyes with FLEX technology and only after that he gets permission to use technology ReLEx SMILE.
By the way, if you are planning a SMILE operation, you can always ask Zeiss if the surgeon has a license for this.
The clinic may not receive a number of licenses. For example, first a new doctor needs to do a dozen training operations on pig eyes, then you can get licenses for FemtoLASIK, after gaining experience - on FLEX, and already after about 70 operations in total - on ReLEx SMILE. Immediately do complex operations, no one will.
- How to reduce the risk of complications?
Here are the main dependencies:
- The quality of diagnosis depends on the risk of keratoctasia and accuracy of correction. The probability of keratectasis can be reduced to a minimum using a number of modern diagnostic techniques for examining the cornea: by keratotogram of the anterior surface of the cornea, according to waveform videograms, by rotational three-dimensional scanning using Pentacam technology, by confocal microscopy, by optical coherent tomography of the anterior eye, using ultrasound scan. But the vast majority of Russian ophthalmologists do not have such equipment.
In addition, the diagnosis determines in general the possibility and prognosis of exactly the method of operation that you will be doing.
Due to insufficiently complete and qualified examination in the absence of the necessary diagnostic equipment, or incorrect analysis of the data obtained, or insufficient knowledge of this pathology, you can simply make a mistake. - The accuracy of the SMILE correction depends on the accuracy of capturing the eye with the cone and setting the marker beam, in the excimer, on the selected mode (taking into account the Eye-traker).
- From the capabilities of the laser (available aspherical profiles, frequency and minimum pulse) - the degree of injury to the cornea, the accuracy of the correction.
- From the psychological skills of the doctor - your peace of mind during surgery.
- From the literacy of all checks on the protocol - the exclusion of accidents.
- From the manual skills and experience of the surgeon - separation and extraction of lenticules, as well as behavior when complications arise during the operation. For example, uncertain surgeons with SMILE corrections often increase the laser's energy level so that the lenticulum goes away more easily and uses increased incisions. This item is closely related to the previous one, including the settings of the operating frequency and the pulse ratio of the laser pulse for the operation.
- From the medications used - reactions after surgery, including the management of regression and the appearance of "heyz."
- From your immunity and the correctness of compliance with the regime - the risks of infection and displacement of the flap (if you did LASIK). And as a result - keratitis, that is, inflammation of the cornea. With SMILE correction, the restrictions are only for a day, for other types of correction - from 2 weeks to a month (do not bathe, do not scratch the eye, do not give the dog a lick of the face).
Here are more details , and here - the consequences of complications and diagnosis.
Thus, with a good diagnosis, even a novice surgeon can perform the operation without difficulty. But if something goes wrong (a chance of 0.5%, I remind you that these are statistics of experienced surgeons), it is better that there is an opportunity to make a further decision together with an experienced colleague. That is why novice specialists do the first 50-100 operations (after training in the pig's eyes) themselves, but an assistant with extensive surgical experience is close by.
Technologically, there are special methods that allow additional correction after laser correction, carried out by any of the existing methods for today - for SMILE, FemtoLASIK, LASIK or PRK. How exactly - decide the doctor.At the European Congress ESCRS in Copenhagen last year, one of the leading refractive surgeons in the world practicing in London, Dan Renstein, gave a report that listed 5 different methods of correction in various cases. So, if the patient suddenly needs, there is plenty to choose from. After SMILE, the quality of optics on 6th generation lasers is consistently higher than after LASIK or FemtoLASIK, the probability of optical side effects is significantly less. When we are planning a laser correction, we expect that this procedure is done only once in a lifetime. The percentage of the correction on the generalized international statistics for SMILE is the lowest today - about 0.5%. In specialized clinics with experienced doctors, it is significantly less. I repeat, specifically, we did not have them, but the probability cannot be ruled out, and therefore - so far, ratherquestion of experience and luck.
- How will the operation go?
Consider the example of ReLEx SMILE.
- You go to the clinic and conduct a comprehensive diagnostic examination, which takes 1.5-2 hours. It is conducted with research on a large number of different devices, including a number of studies conducted with an expanded pupil. Therefore, it is better to choose a convenient day for you and arrive by public transport. A week before this, it is desirable to remove soft contact lenses (hard - for 2-4 weeks), since wearing lenses affects the results of some measurements. One day to make the diagnosis and correction will not work - you need to wait for the constriction of the pupil. The next day, you can prescribe the operation, if after consulting the surgeon there are no contraindications for it.
- , , , , , , . – . , – . . .
- , , . , , . .
- , , -, . . , . – , . . , , .
- – , . – , . , , . , ( ). – . - , «Ready!» ( «!»). , – . , , 26 ( ). Like this:
- , – , . - , , .
, . , , . – .
Here there are details about how the laser works - if very briefly, it creates a focusing point in the thickness of the cornea, a microexplosion occurs there, then a cavitation bubble forms and the plasma gently pushes the tissue around the focus point. A chain of such pulses forms a res.
Here is more detailed about the course of the operation and what you will see. About related questions - here .
The operation on both eyes takes 10-15 minutes.
- What you need to know about the cornea?
The cornea is the most complex formation that is formed in embryogenesis from three different types of tissue: surface ectoderm (epithelium develops), mesoderm (stroma) and neuroectoderm (endothelium is formed). As it develops (differentiated), each of these tissues needs the isolation provided by boundary shells to preserve its structure and specificity. Thus, the endothelium forms the Descemets sheath, and the stroma - the Bowman's sheath. Here is the diagram:

1. corneal epithelium; 2. Bowman's membrane; 3. corneal stroma; 4. Descemetov shell; 5. corneal endothelium.
The corneal epithelium is a multilayered tissue, cells in 5-7 rows. It protects the eye mechanically, does not let microorganisms and small mote, provides an immune response. Mucin of the tear film fills all the irregular elements in the surface epithelium, which provides a smooth transparent surface. Like the normal epithelium of the skin, it regenerates well, and during PRK surgery it is removed to gain access deeper. Within a few days, it is restored.
The second layer is the Bowman's membrane. This is a thin layer immediately below the epithelium. Does not contain cells, consists of randomly arranged collagen fibrils. Some animals do without it in principle. In humans, at least performs the function of compensation of intraocular pressure and a number of other tasks that are not yet fully understood. The Bowman's membrane cannot be restored after damage, therefore, after corneal damage in this part, scars are formed at the site of defects and the transparency of the cornea in these areas is disturbed and turbidity is formed. When laser correction lenses are formed deeper. However, at any cut through the bowman's membrane, we cut the nerves, of which there are quite a few. In PRK, the membrane is removed entirely to gain access to the stroma. Just in the Bowman's membrane, which, due to congenital or acquired inferiority, ceases to perform the barrier function, keratectasia begins.
With minimally invasive removal of lenticules with ReLEx, there is only one short cut (2.5 mm), and not nearly the entire circumference, as in the case of LASIK / FLEX-like methods. It is damage to the Bowman's membrane that disrupts the epithelization of the eye, innervation, and other side effects.
The next part of the cornea is the stroma. This is where the main work goes. Fabric - collagen filaments impregnated with hyaluronic acid. When magnified, they resemble ropes. These parallel plates are formed from collagen fibrils. They know how to merge. If the ropes stick one into the other, then with the formation of nodes-adhesions, and this prevents visual acuity.
But, being laid on each other overlap (that is, from different angles), they do not form these knots, but simply interlock. During the laser correction ReLEx SMILE we cut the lens in this layer and remove it. After the operation, the cavity in the cornea closes in - the “ropes” lie on top of each other, but at the sites of the incisions a clear boundary does not form from the joints, that is, everything remains transparent (splices of single collagen filaments occur at the border of the lens, that is, in outer diameter). The skeleton is supported as usual - with the Bowman membrane stretched from above and the lower layers.
The next two layers — the Descemets membrane and the endothelium — have little interest in laser correction, since we are not affected by these operations. This is actually a soft and hard boundaries of the body, a kind of standard "casing" for the body.
- “Glass Worms”, which are DST, what about them?
With them is a completely different story . In short - in most cases you don’t have to touch them, the risks of complications, laser shooting of the vitreous body are still there. But if they are very dense and interfere (for example, one of the truckers complained about a “blizzard in the eyes when braking”) - you can correct it. Only a specialist can decide whether to work with a laser or have an operation. Surgery - vitrectomy (removal of the vitreous body). It is quite serious in depth of penetration - as the retina is located near, it refers to high-tech types of operations.
The risk to benefit ratio is always strictly evaluated.
- What you need to know about the price?
Prices for laser vision correction may vary significantly. First of all, first of all, the cost depends on the chosen correction method, since this, in turn, is determined by the cost of the license of the manufacturer (the license for SMILE or IRC is much more expensive than FLEP). All modern lasers have licenses to perform a certain type of correction - for example, personalized LASIK is sold under separate more expensive licenses than the standard LASIK.
The old antediluvian lasers (excimer and femtolasers of the old generation) did not have a license, but performed a poor quality correction. Until now, many clinics work for them - these are just options for “Buy a coupon” or “Discount - 50%”, because these obsolete machines have paid for themselves for a long time, but the equipment is not updated.
Secondly, of course, there is a dependence on the region, on the country, etc. For example, in our SMILE EYES Augenklinik Moskau department, the cost of correcting the vision using the SMILE method agreed in the holding is cheaper than in Germany and Austria. We have 105,000 rubles for the cost of one eye - at a price of 2,500 euros (175,000 rubles) in European offices.
By the way, Professor Sekundo from Germany operates in Moscow at the European price, but his patients save on travel and accommodation when choosing the Moscow branch. And, for example, in the UK the leading refractive above the mentioned surgeon costs three times as much. But in any case, this high-tech micro-invasive method all over the world is quite expensive and is not covered by insurance. If it is offered cheaply, it is probably for the surgeon or for the clinic the starting point. Or the results of mass surgery are not good - SMILE, like no other technique, is individual.
Thirdly, there is a dependence on the obligations that the clinic assumes. For example, the standard in SMILE EYES in all branches, including our Moscow branch, is a guarantee for observation during the year and potential correction, which is possible in the unlikely case.
Fourthly, there are such clinics where such cost as “presence of astigmatism”, “thin cornea”, “difference between the eyes”, etc., influence and additionally pay for the cost. As a result, the initially declared cost increases significantly. In my opinion, this is wrong. The SMILE procedure takes 26 seconds, regardless of minus and astigmatism, the thickness of the cornea also does not affect, even strabismus does not affect! In these cases, either the surgeon does not understand what he is doing, or this is a commercial trick.
Fifth, the cost is influenced by which surgeon performs the operation. In our clinic, these operations are performed by professors, young doctors do not make this type of correction. Let me remind you that the company Zeiss certifies each surgeon (and often it happens that a license is for one, and performs another under his last name - it makes sense to check before choosing a surgeon). In some clinics there is a surcharge for surgery by a professor, “just a doctor or cms” is cheaper - this depends on the policy of the clinic.
In any case, I believe that laser vision correction is a great investment in your health and quality of life.
- In the end, how best to prepare for the correction?
If you have decided that you need correction, then you need to start with a comprehensive diagnostic examination in order to understand whether you have any contraindications and which method will be best for you.
It is important that the clinic where you are applying has the full range of technologies: the possibility of SMILE, FemtoLASIK, sometimes just LASIK or even PRK is needed. Because if there is no clinic, for example, a VisuMax laser and a doctor who can work on it, then SMILE, alas, will not offer you, but will only recommend what is available and tell you what is best for you.
If there is no femtolaser, they will say that LASIK (for example, super-LASIK or epi-LASIK is the pinnacle of evolution!). Unfortunately, not a single clinic, even with a “killed” laser and “killed” diagnostics, writes that it has “old equipment” - you have to either trust or check.
By the way, data from other clinics can be used for preliminary consultation on the choice of technology and the possibility of correction (if they are in full).
The clinic, which will carry out the correction, is obliged to conduct a full examination on your own - in such a case as surgery, you can not rely on other people's research, everything must be rechecked.
So, first of all, it is necessary to undergo a comprehensive diagnosis in the clinic, in which there is the maximum of all modern correction technologies. If you are using contact lenses, it is advisable to switch to glasses for 1-2 weeks before the diagnosis.
Diagnostics in time is usually not a quick process, takes 1.5-2 hours and after that options of technologies that suit you are offered. In the case of SMILE, the "cherished" global 0.5% of complications on the 6th generation can be reduced to 0.1-0.2% simply due to a comprehensive diagnosis.
Pre-domiciliary, you can take the necessary set of tests recommended by the Ministry of Health of the Russian Federation (we give out the list) or you can do this in our clinic.
You need to come to the surgery without makeup and smelling perfume. Alcohol is better to exclude from the dinner menu the day before.
You need to take your passport and sunglasses with you; you will receive all the accessories you need for the operation in the clinic.
On the day of surgery, special preparation is not necessary, as a rule, you spend a couple of hours in the medical center and then go home yourself. Maintenance is not necessary, the eyes will see quite well (on average, 3-5 lines on the table) within an hour after the operation.
But we prohibit independently driving, you can only drive a car the next day after the operation. It is better not to plan anything serious on the day of the operation, to rest and put off important matters.
The next day you can walk, ride a bike, engage in active sports, usually wash. Immediately after surgery for a couple of hours, you may experience discomfort (from light cramps to moderate tearing) - this is a normal reaction of the body to damage to eye tissue. These symptoms are strongly pronounced after FemtoLASIK or LASIK and an order of magnitude less after SMILE.
After PRK, the pain will persist for two weeks - this is not the most pleasant operation. The next day after surgery, you are monitored by a doctor, then after a week or two. The next inspection is in 3 months, then in 10-12 months.
If you have any unplanned questions - you can always make an appointment and come for a visit to dispel your doubts. You can write by e-mail - your doctor will answer you. But we must remember that, not seeing you, the doctor can not make a diagnosis by phone or change the treatment regimen.
Operations on two eyes are done on the same day. In theory, of course, you can spread for several days, but it is inconvenient and has no medical indications.
Another point - after correction, people in many professions (for example, chemists, cooks, etc.) need to be careful if they have worn glasses before. During the years of wearing glasses over their eyes, they have the feeling that you can bend your head directly over the pan or not wear special protection in the laboratory. After the correction, it takes several weeks to get used to the fact that the oil from the frying pan is splashing, and protection is needed in the chemical laboratory.
- How does the correction for boys differ from the correction for girls?
Nothing. The eyes of men and women are the same, the risks too. Let me remind you once again that pregnancy and the feeding period for girls is a time when the correction cannot be done. I recommend to return to the question of correction 6-8 months after the end of lactation.
By the way, for medical reasons, laser correction can be done at an earlier age.
The recommended age for correction is from 18 years and older, but there is no age limit in a big way. But all, of course, individually.
- What correction do?
The doctor will tell. SMILE is an advanced technology that has enriched the repertoire of laser-refractive surgery to make them even safer and more comfortable. The question should not be that it is good, but that is bad, but that an individual approach is needed. And each method has its pros and cons. If the patient is young, and even the cornea is thinner, then undoubtedly, the best technique is SMILE, because there is less risk of keratectasis, more stability of the achieved effect and excellent vision the next day with phenomenal comfort. The same for a person at the age of 50 is easier to treat with FemtoLASIK (it does not mean that it is better): the cornea is harder (less risk of keratectasia), and the next day it will probably see better than after SMILE, because a hard cornea needs more time adaptation of the internal slice. A dry eye, of course, will torment longer, but after six months the difference is gone. Well, if you need an economical option, then PRK will also give an acceptable result with a little myopia. Therefore, FemtoLASIK, SMILE and even PRK (especially for refractions in the region of 1 diopter) are able to exist next to each other.
Ordinary LASIK, this excellent operation by the standards of two thousandths, today needs to be done in exceptional cases (for example, scars in the cornea). Despite the persuasion and all advertising words - the other options are better. In your particular case, most likely, the relief features of the cornea’s surfaces and its thickness, profession and hobby, age and much more will fall on this picture - advice is useless without diagnosis.
- What does an IT specialist need to know about vision?
Let's start with platitudes: the less you sit at a computer, the better. The more often you relax and look away, the better. If you are fond of sports such as table or tennis, or badminton, or golf, etc. (where there is a frequent change of focus) is good. Of the average importance of things - watch the light, it is best to use indirect light (for example, a lamp with a lamp shade) so that it is dim and not quite dark. Do not put the monitor so that there is a glare, use matte screens, if you can. There is almost no difference in reading from a tablet or an e-book (there is no research, I can’t justify with numbers), but subjectively - from a well-lit screen, e-ink is better.
The most important thing: if you have a screen at your workplace or at home 13-17 inches, then you can improve your life if you buy a larger display and place it a little further away than the current one - at least 10 cm. And better by 20. Not move the monitor closer to you when reading small text, and increase the font size if you can transfer it comfortably for reading speed.
Rest, take short breaks, leaving the computer: at lunch, go for a walk, and do not sit at the computer, do not be lazy to go to the printer or have a cup of coffee.
There are no clinical data on different types of screens and their flickering, problems were only with screens based on cathode-ray tubes. So, if you work at a computer, and especially from a laptop, it is better to do it at the table, sitting straight and level (this ensures that there are no problems in the cervical spine, that is, as a result, a normal blood supply to the head), often get up and watch out the window.
Long-term work at the computer leads to a violation of the stability of the tear film and to the appearance of such a disorder as “dry eye syndrome”. It is necessary to blink more often or use special moisturizing drops, or put a humidifier.
In general, the eyes of an IT specialist are exactly the same as other people. For an adult, the danger of working at a computer is greatly exaggerated. There is no particular difference between what you would read 8-10 hours a day in the eighteenth century or sit at a computer today.
But, let me remind you, in the eighteenth century, general surgeons provided eye health, there were no antibiotics, ophthalmology was only in its infancy. You are definitely lucky with the twenty first century. But most importantly, you can be calm about the need to change jobs. If you follow the rules - everything will be fine.
Everything!
Seems to be able to answer all your questions in one place. If there is more - ask, I will update the FAQ.
More of our posts, where everything is more detailed:
- Laser that cuts inside the cornea: ReLEx procedure at the physical level
- Laser telemetry for vision correction: a complete operation with comments (not for the faint of heart)
- History of vision correction operations: comparison of risks and side effects
- A couple more unobvious things that you might not be told before laser vision correction
- FAQ about laser correction ReLEx SMILE: yes, in Russia there is, but no, in Russia there isn’t
- We got to the side effects of laser vision correction and more - to diagnose
- Vision correction equipment
- "Augmentation" eyes: what we build into it today and what else remains under it
- Calculation of intraocular phakic lenses (embedded in the eye) - we continue about the eye and its biomechanics
- What is more dangerous: wearing contact lenses or laser correction?
- IT specialist's vision: what you personally need to know
- Keratoectasia (keratoconus, "bulging cornea"): what is it and what to do with it
- Cataract: it is waiting for you personally (if you live, of course)
- We implant an artificial lens (you will need it after 60 years)
- How do doctors do the vision correction themselves
- Keratoplasty - the last option to “fix” the eyes, if everything is bad (and something about modern methods)
- Night contact lenses for those who do not wear glasses, but are afraid of this correction
Source: https://habr.com/ru/post/370705/
All Articles