Blood cells on the chip will allow you to learn more about thrombosis and their treatment.
It takes an average of five billion dollars to bring to the US drug market, of which 60% is spent on research. Using models of human organs will reduce costs and reduce the cost of development, and the lack of the need to use experimental animals will make testing drugs for humans more effective.
The organ-on-chip technology was created at Harvard . Researchers reproduce the micro-architecture and functions of living organs, the list of successful experiments includes the heart, lungs, intestines. Each chip consists of a transparent polymer, has the size of a flash drive and contains hollow microchannels, in which living human cells are located.
In March 2015, the University of California at Berkeley created a heart on a microcircuit : living cells pulsate and respond to drugs. Scientists "packed" cells with a microcircuit, the cells formed a tissue and after a day began to pulsate with a frequency of 55 to 80 beats per minute - this is the normal pulse of an average adult person. When the heart was affected by isoproterenol, the pulsation increased.
')
Emulate, Inc. develops the harvard concept. The next step is “thrombosis-on-a-chip” : the models mimic the factors leading to the formation of blood clots. Clots can stop bleeding from a small wound, but rapid blood clotting can block the flow to the organs - the brain, the heart and the lungs.
Deep vein thrombosis is characterized by the formation of blood clots in deep veins, most often in the lower limbs. The disease occurs in 10-20% of the population and, if left untreated, causes up to 15% of deaths from pulmonary embolism. The study of blood behavior will help pharmaceutical companies to come up with more effective ways of treating such diseases. The chips will allow you to test new treatments without harming sentient beings.
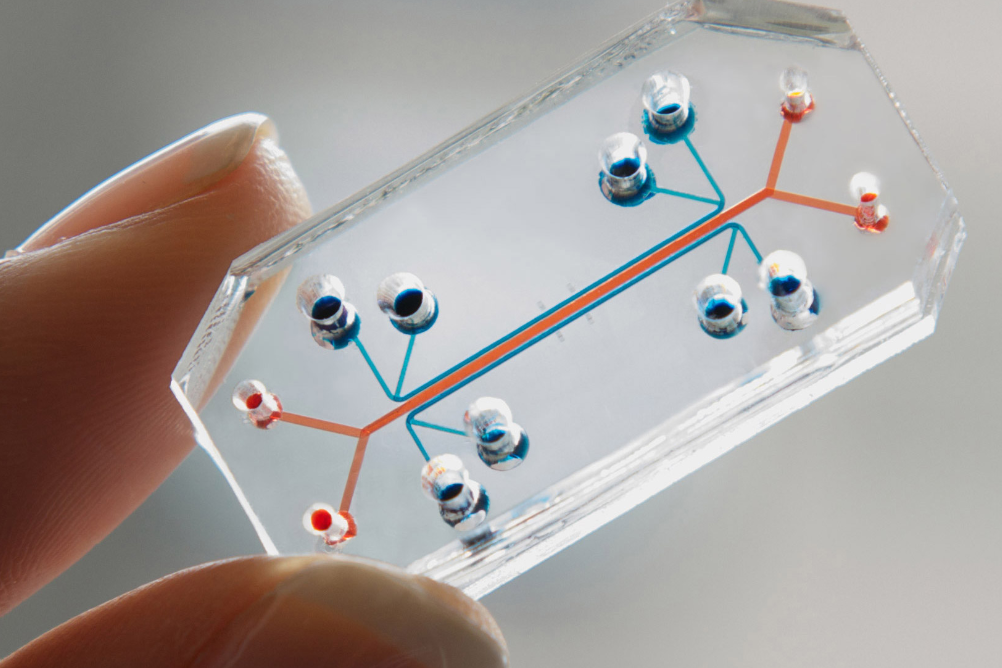
The organ-on-chip technology was created at Harvard . Researchers reproduce the micro-architecture and functions of living organs, the list of successful experiments includes the heart, lungs, intestines. Each chip consists of a transparent polymer, has the size of a flash drive and contains hollow microchannels, in which living human cells are located.
In March 2015, the University of California at Berkeley created a heart on a microcircuit : living cells pulsate and respond to drugs. Scientists "packed" cells with a microcircuit, the cells formed a tissue and after a day began to pulsate with a frequency of 55 to 80 beats per minute - this is the normal pulse of an average adult person. When the heart was affected by isoproterenol, the pulsation increased.
')
Emulate, Inc. develops the harvard concept. The next step is “thrombosis-on-a-chip” : the models mimic the factors leading to the formation of blood clots. Clots can stop bleeding from a small wound, but rapid blood clotting can block the flow to the organs - the brain, the heart and the lungs.
Deep vein thrombosis is characterized by the formation of blood clots in deep veins, most often in the lower limbs. The disease occurs in 10-20% of the population and, if left untreated, causes up to 15% of deaths from pulmonary embolism. The study of blood behavior will help pharmaceutical companies to come up with more effective ways of treating such diseases. The chips will allow you to test new treatments without harming sentient beings.
Source: https://habr.com/ru/post/367435/
All Articles