Part 4.2 We return the sight. From points to the excimer laser
Guys, there is a laser. He bites into your eye. But earlier, so that the laser could start work, it was necessary to carefully clean the eye with a scalpel. The scalpel over time became smaller, and the laser - steeper. Therefore, let's look at the evolution of methods.
Epigraph from Milfgard

The final part of the cycle, devoted directly to the remaining methods of vision correction. In this part, we will look at orthokeratology, all variants of laser vision correction, lens replacement, and several other methods. If you have not read the cycle from the very beginning, I highly recommend that you familiarize yourself with parts 2 and 4.1, which examine in detail the problems faced by the modern eye surgeon. In this article I will try to dispel the already tired fear associated with the film "Destination 4" and the laser gone mad. Also, I will try to answer the questions posed by readers, as promised.
')
Previous parts
Part 1. Unboxing VisuMax - femto laser for vision correction
Part 2. How many megabits / s can be passed through the optic nerve and what is the resolution of the retina? Some theory
Part 3. Meet - laser called Amaris. Moving and first awakening of VisuMax
Part 4.1 We return the sight. From points to the excimer laser
Table of contents:
We change the cornea
- History: Radial keratotomy
- Mow the lawn or how to get to the working area
- PRK and trans-PRK
- Lasik
- femto-LASIK
- ReLEx SMILE
- ReLEx Flex
- Orthokeratology
When the cornea is missing
- Phakic lens implantation
- Implantation of an artificial lens - IOL
We change the cornea
Having exhausted all the possibilities of temporary correction of vision with various lenses, we turn to the techniques. which will allow you to permanently withdraw points. Most often, the indication for laser vision correction is the desire of the patient himself to get rid of glasses. Sometimes these are medical conditions associated with complex types of astigmatism and myopia, which are difficult to correct in other ways. There are many techniques, but they all boil down to changing the shape of the cornea in order to correct the refraction of light.
For a more complete understanding of the techniques refer to the structure of the cornea.
The first protective barrier between the tissues of the eye and the external environment is the anterior epithelium . It is transparent and passes oxygen to the underlying layers. The scheme of its update is very interesting. The epithelium is actively divided on the periphery of the cornea and gradually migrates to the middle, where it ends its cycle, peeling off.
Photos of mutant mice illustrating epithelial regeneration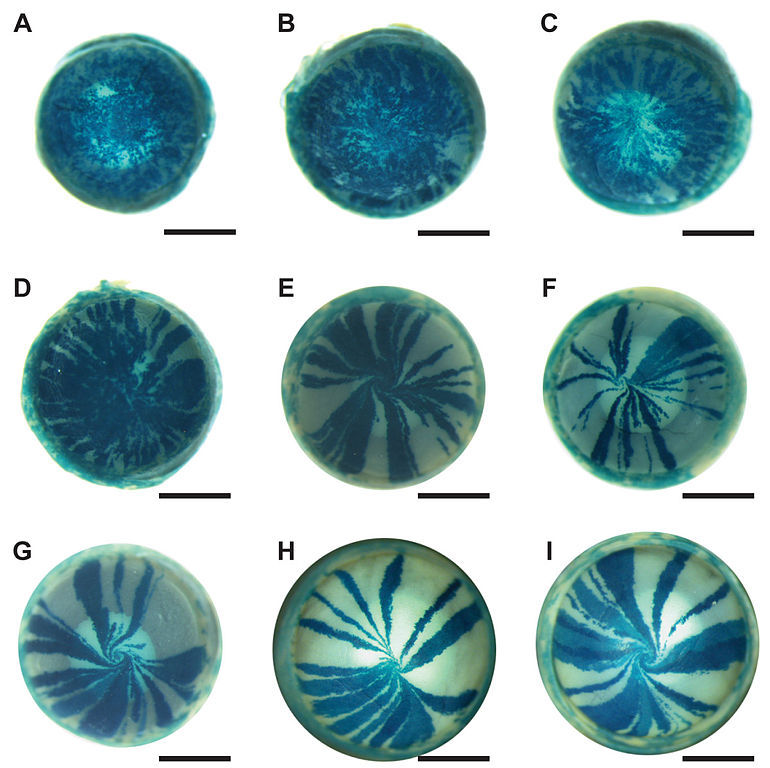
"Mosaic analysis" of epithelial cell renewal in the mouse eye. Applied staining using the reporter gene encoding the protein beta-galactosidase. Half of the mouse body cells in this model express the XLacZ transgene, half do not. In the photographs of the eyes of different "mosaic" mice, one can observe how the new cells are moving towards the center, creating a small "whirlpool". A: three weeks after birth, stem cells are just starting to activate; B: 6 weeks; C: 8 weeks; D: 10 weeks; E: 15 weeks; F: 20 weeks; G: 26 weeks. Fragment of illustration from Mort et al., 2009.
"Mosaic analysis" of epithelial cell renewal in the mouse eye. Applied staining using the reporter gene encoding the protein beta-galactosidase. Half of the mouse body cells in this model express the XLacZ transgene, half do not. In the photographs of the eyes of different "mosaic" mice, one can observe how the new cells are moving towards the center, creating a small "whirlpool". A: three weeks after birth, stem cells are just starting to activate; B: 6 weeks; C: 8 weeks; D: 10 weeks; E: 15 weeks; F: 20 weeks; G: 26 weeks. Fragment of illustration from Mort et al., 2009.
The next layer is the Bowman's membrane . Its functionality is still unclear. Moreover, this layer is simply absent in some mammals. After damage is not restored. Cell does not contain.
The most important layer in terms of vision correction is the stroma . The stroma is formed by a variety of lamellae - parallel plates arranged woven from collagen fibers. It is this layer that undergoes partial evaporation with laser methods of vision correction. Achieving a stable result due to the stability of this layer. Precisely because the layer lies under the epithelium, to achieve it, it is necessary either to completely remove the overlying layers (PRK) or to lift them in the form of a flap-flap (LASIK, femto-LASIK)
History: Radial keratotomy
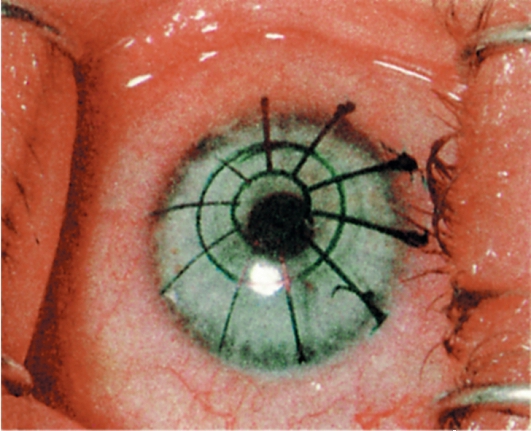
Corneal marking before incisions
This method is currently of purely historical interest. The use of corneal incisions began at the end of the 19th century. The newest myopia surgery was created on the basis of ideas and experiments of prof. Tsutomu Sato of Tokyo University (Tsutomu Sato of Juntendo University, Tokyo). He noted that the spontaneous breaks of the Descemet's membrane in keratoconus lead to a flattening of the cornea after their healing. This was the basis for the formation of the idea of the posterior corneal incisions. He also noticed that damage to the eye from the Descemet's membrane is much more traumatic than that from the Bowman's membrane, but more effective. Later, in the 1940s, front incisions were introduced as an addition to the posterior incisions to enhance their effect after an experimental study of tangential corneal incisions in rabbits. Surgery for myopia in patients began in Japan in the early 50s.
After the death of Sato and his followers, myopia surgery in Japan began to decline and resumed in the USSR. Soviet ophthalmologists have come to the same conclusions. What Sato. The front radial cuts were not as effective, they ultimately concluded that the length and distance from the limb, as well as the depth of the incision, determine its effectiveness.
From 1970 to 1980, S. Fedorov and his colleagues made a significant contribution to the development of radial keratotomy technique. Interest in the operation technique brought the flow of American ophthalmologists to Moscow. At that time, he reported 99% satisfactory results of the operation and he said that he had no more than 1-2 complications per 1000 operations.
Later it turned out that the method has significant complications in the case of eye injuries received after the correction. So, as the incisions for this method significantly violated the architecture of the cornea, in the worst case after the injury there were massive gaps along the incision lines. "Collect" the cornea in a normal state after this was extremely difficult. Currently, the method is superseded by much safer and more physiological LASIK / femto-LASIK.
Mow the lawn or how to get to the working area

When I tell employees about the differences between the LASIK and PRK options, I call for the following metaphor for help:
Imagine that you have a nice dense lawn. But, by a strange coincidence, it is under him that there is a very necessary technological hatch with which you need to work. Lawn you want to keep in good shape. You have two options:
- Make a careful cut around the hatch and raise the sod. In this variant, the roots and stems along the perimeter will be crossed, however, the grass will very quickly overgrow this seam. Grass on raised turf will remain untouched.
- Shave trimmer and dig the ground over the entire area above the hatch. Over time, the grass will grow back on the mowed area, but it will be much later.
So, as many have already guessed, the grass symbolizes the corneal epithelium, and the two methods LASIK / femto-LASIK and PRK, respectively. Accordingly, in cases with flap, the corneal epithelium remains alive, and the PRK variant, although it allows working with a very thin cornea, is distinguished by a long recovery period for epithelial regeneration.
PRK - photorefraction keratectomy
With this method, the cornea is evaporated by a laser after the removal of the top layer of tissue by chemical or mechanical means. This method does not provide for the creation of a flap flap, which allows its use with a very thin cornea. The method has a rather narrow application due to its difficult side effects and difficulties:
- The potential for corneal opacities is Haze
- For girls you can not become pregnant for a year, use hormonal contraceptives
- Long recovery period, often more than a month
In general, the method is applied only for very narrow indications. There is a variation - trans-PRK, in which the upper layer evaporates with a wide beam (wide-aperture laser). In any case, with this method, the Bowman's membrane is irreversibly removed. The epithelium is restored naturally over time.
LASIK - Laser-Assisted in Situ Keratomileusis
The classic method that for many years. A distinctive feature is that a special blade is used to remove the flap - a microkeratome. Fixation of microkeratome is provided by a zone of reduced pressure. This method is more traumatic than its evolutionary continuation - Femto-LASIK. Moreover, ordinary LASIK is prohibited in several countries, as outdated, for example in Italy.
Femto-LASIK
One of the most popular methods at present, along with PRK. In contrast to PRK, the epithelium and Bowman's membrane is preserved in integrity. As a result, recovery time is minimized. The risk of infection is minimized, since mechanical tools for flap formation are not used. It becomes possible to plan an individual flap profile, rather than averaged in shape, as with a regular LASIK. This makes it possible to design the operation in an optimal way, resulting in high-quality vision.
In order to form a flap, the first of the lasers begins to form a slice at a predetermined depth. This is due to the evaporation of tissue under the beam. As a result of such exposure, a gas bubble with a diameter of 2 microns is formed. The distance between the individual bubbles is 3 µm, and the distance between the coils of the helix is also 3 µm. The energy per shot is 130-170 nJ on average. The accuracy of the work is the highest. Individual parameters are regulated depending on the specific situation and may vary within certain limits.
We are very proud of our Amaris excimer laser, primarily because of its safety and a variety of operation control systems. In previous articles, many wondered what would happen if the patient twitches, the lights go out, and the like. Consider the software and hardware implementation:
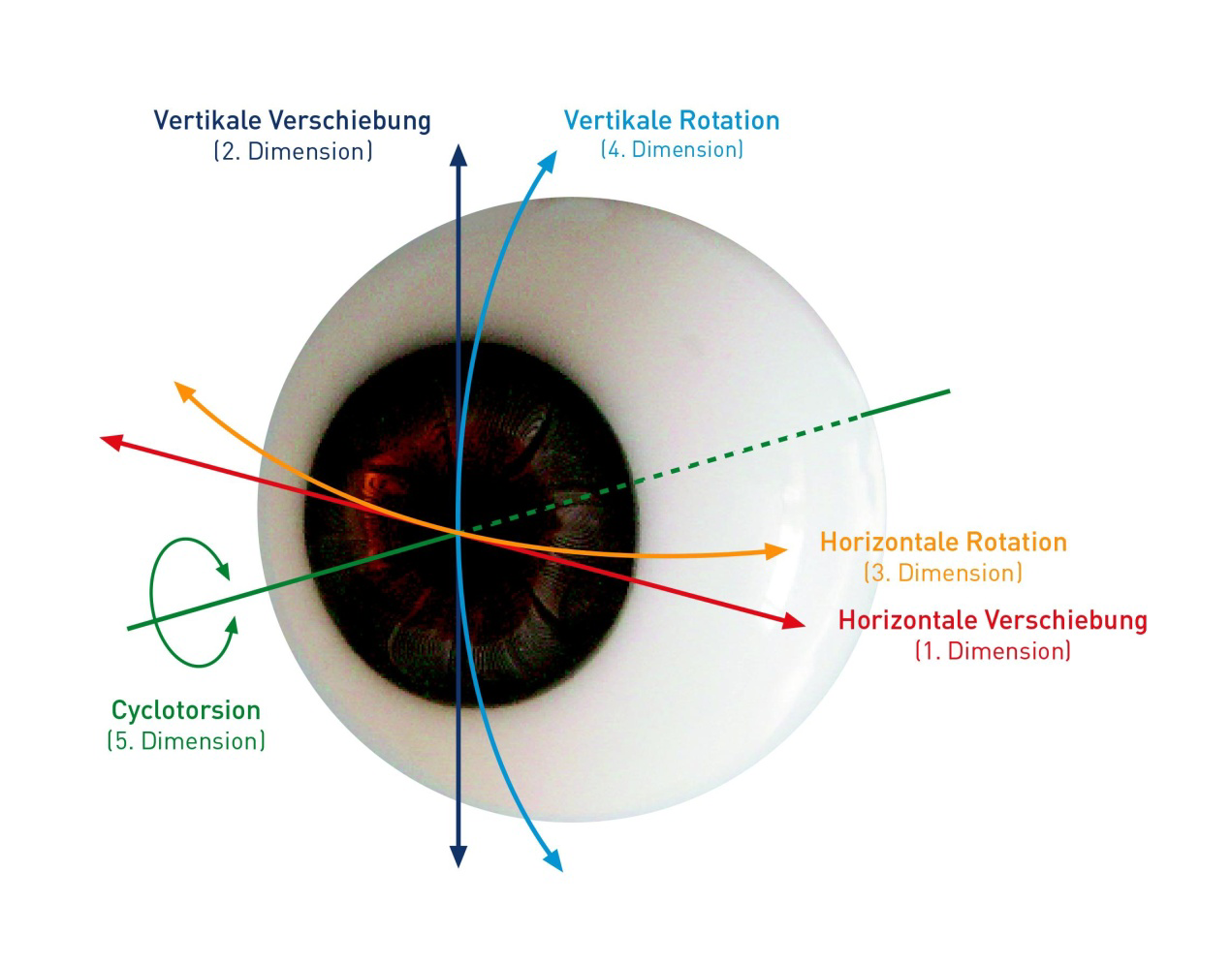
Control the movement of the eye in five directions, including rotation. Before the operation begins, a comparison of the image of the iris and a given program of cornea evaporation takes place. In the process of automation controls the procedure and specifies the coordinates in which the laser operates dynamically. The reaction time to change the position of the working area is not more than 3 ms. If the eye is too displaced relative to the working position, the procedure will be automatically interrupted.
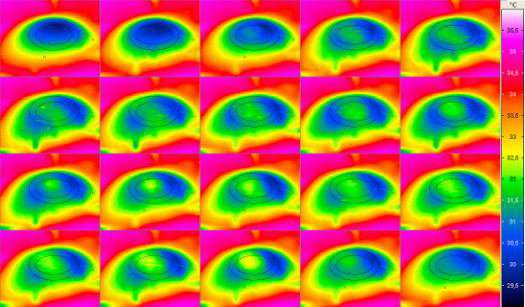
A special sensor continuously monitors the temperature of the surface of the cornea, preventing its damage due to overheating.
In the video you can see a system for optimizing the power of the laser beam. Initially, the laser operates in the mode of high-energy pulses, which allows you to quickly form the desired curvature of the surface. The remaining 20% of the time, the laser operates in a low-energy mode, achieving perfect surface smoothness. As a result, the system allows you to quickly and accurately remove a strictly specified amount of corneal tissue.
ReLEx Flex
ReLEx Flex technology. The general principle is to cut out the flap using a single Femto laser. Then, after folding off the surface layer, the second flap is removed as a page from the book. As a result, the cornea changes its shape as needed.
ReLEx Smile
ReLEx Smile technology. Also performed by a single femto laser. The peculiarity of the method lies in cutting out the lenticular flap in the thickness of the cornea, which is then carefully removed with tweezers through a thin incision. As a result, the cornea is flattened in a given manner and refraction returns to normal.
Orthokeratology

Orthokeratology is a technique that declares the correction of refraction by wearing special hard contact lenses. The essence of the method is in the gradual deformation of the cornea with these lenses according to a previously calculated pattern. I was repeatedly asked about the effectiveness and safety of this technique. After consulting with the collective mind of our colleagues, we came to a number of conclusions:
- The technique is very young and there are no long-term results. The same LASIK with all its innovations like femto technologies has long been studied in more than 20 years of observations.
- The technique is supposedly aimed at reducing the cost of correction and lowering the threshold of entry into this business. For its use only keratotopograph and machine for milling lenses are needed. That is, we are immediately saving more than 40 million rubles for equipping the operating room with modern lasers. Moreover, there is no need for a full-profile clinic and the opportunity to work almost in the format of a pharmacy / optics in a small room. Naturally, it is attractive to many who promote this business model.
- The duration of the effect of correction is very doubtful. With this technique, the change in the shape of the cells of the cornea under the influence of the hydraulic influence of the lens is declared. However, the long-term effect is doubtful several years after the cancellation of the lens exposure.
- Even the usual wearing of lenses is not at all useful for the cornea. An additional deforming effect can potentially lead to serious complications such as keratitis, disruption of the structure of the corneal epithelium.
- Moreover, it has already been mentioned about the danger of wearing lenses at night, when the eyelid is closed, and oxygen for the cornea is supplied in a minimum amount. Rigid contact lens will significantly worsen the situation and cause chronic oxygen starvation of the corneal tissue.
Summarizing: our clinic does not deal with this area, considering it inexpedient and controversial. All this does not prevent others from having an opinion different from ours.
After correction
Limiting visual loads
After surgery, it is recommended to avoid excessive visual loads in the first few weeks. The eyes and brain need time to adapt to the new refraction. In fact, it is not uncommon for a patient to undergo an examination on Thursday, operate on Friday, and on Monday he does not take his eyes off the monitor in the office. Of course, doctors like this do not approve, although the current rhythm of life dictates its own conditions.
Limitation of physical activity
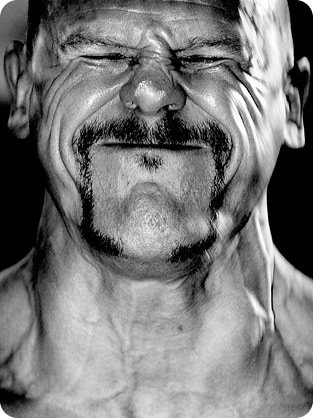
The first month after the operation, it is necessary to minimize physical activity, gradually reaching the usual level by the end of this period. After a month of physical rest, you can play sports in the usual rhythm, as before. It is necessary to remember a very important thing - the diagnosis of myopia does not disappear anywhere after correction . That is, a person remains short-sighted with a distended eyeball, but at the same time it will be well to see. The increased size of the eye is fraught with the risk of retinal detachment, which is not able to stretch as much as other tissues. Accordingly, a myopic person, both before and after the correction, will not be able to lift weights and overstrain. The reason is a sharp increase in arterial and intraocular pressure during forced loads. In order to understand it is better to just look at the photos of weightlifters during the breakthrough:

When not enough cornea
Possible points of impact
Unfortunately, there are situations when the cornea is too thin even for PRK, and for medical reasons a person really needs a correction. For example, the big difference in diopters between the eyes may not allow a person to wear glasses. A man cannot do without correction either. Then backup technologies come to the rescue, with their pros and cons. Naturally, such operations are not shown to everyone.
Phakic lenses
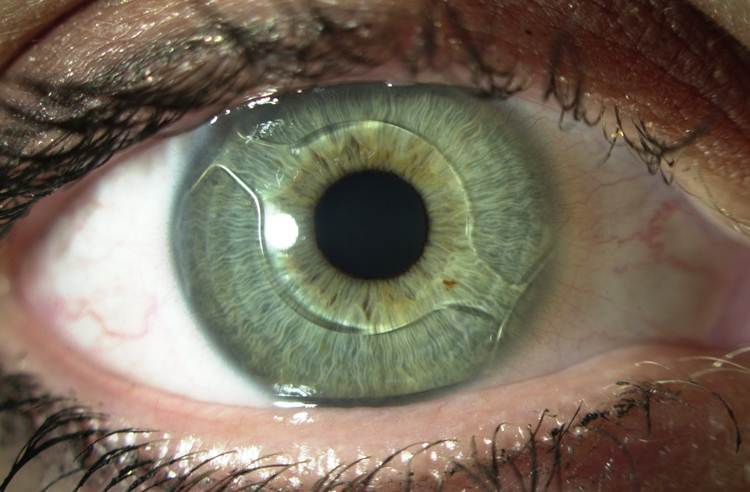
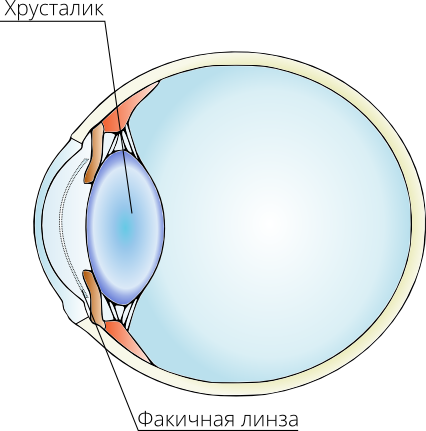
One of the possible options for the correction of refraction in a situation of a very thin cornea is the use of phakic lenses. Transparent lenses adjust the light beam to compensate for refractive errors. They are usually applied at high values of myopia / hyperopia, if it is impossible to correct the refraction due to the cornea. Have fairly limited readings.
There are three types of phakic lenses that are implanted to correct refractive errors. Their name is determined by the location in the eye: anterior chamber phakic lens, iridofixation phakic lens (with fixation to the iris) and a backcameral phakic lens.
Appearance fakichnoy lenses
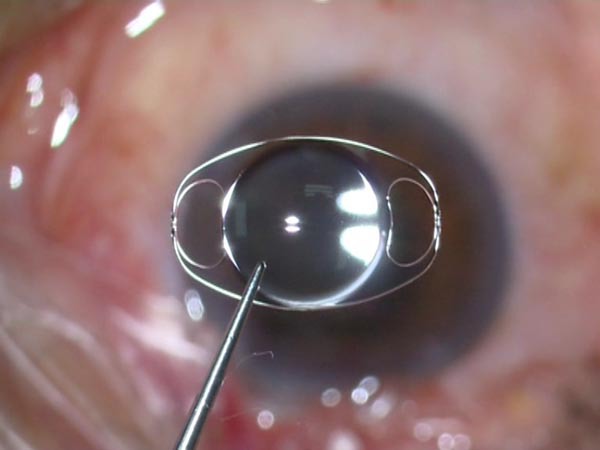
Lens replacement

In the illustration, the doctor packs an artificial lens into a special injector before implantation.
This technique is in itself a separate article. Most often, the lens is replaced because of its clouding due to cataracts. However, the replacement of the lens can also correct refractive disorders. Accurately calculated lens can compensate for both astigmatism and pronounced myopia / hyperopia. Naturally, the artificial lens does not have the ability to change its shape, which means there will be no accommodation. The method also has limited indications, but can be a salvation for some categories of patients.
We answer questions
In past articles I was asked a lot of questions - under the spoiler, I will try to highlight those moments that were not disclosed in past articles.
Spoiler

As far as I know, there is no evidence of a positive or negative effect of wearing such glasses. Theoretically, they can contribute to the removal of spasm of accommodation, but is hardly more effective than special drugs. The concept of these points was extremely popular in the 90s, and even now they are trying to sell them as a miracle cure “from everything”. The principle of operation is almost identical to the principle of pinhole . With a very small hole, the depth of field tends to infinity.
Punch glasses

As far as I know, there is no evidence of a positive or negative effect of wearing such glasses. Theoretically, they can contribute to the removal of spasm of accommodation, but is hardly more effective than special drugs. The concept of these points was extremely popular in the 90s, and even now they are trying to sell them as a miracle cure “from everything”. The principle of operation is almost identical to the principle of pinhole . With a very small hole, the depth of field tends to infinity.
UPD Dare 's Photo Report of the operation

The first day after surgery) Habravchane not often come to us as patients. Phoned to the patient - he feels well. Medical phone bypass)
He shared his impressions on his blog: Vision correction through the eyes of a patient
I also highly recommend his previous entry on diagnostics and equipment - Do not shine a laser in the eye!
On the equipment for the diagnosis will be a separate article detailed a little later.
Source: https://habr.com/ru/post/219735/
All Articles